Introduction
Problem
The Outpatient Department (OPD) of Al Hada Armed Forces Hospital - Taif Region (AHAFH) is composed of 40 specialized services and subspecialties, supported by 120 rooms (85 clinic rooms, 18 procedure rooms, and 17 vital signs rooms). As a tertiary hospital offering specialized services, challenges may arise in providing timely access to these clinics. To address this issue, it was crucial for us to understand the patient flow process, supply and demand, and the mechanism behind queuing.1
Numerous studies are available describing challenges and methods to address issues related to access in outpatient departments. This project was initiated from the General Directorate for Health Services at the Ministry of Defense (MODHS) in early 2020. In the last few weeks of fourth quarter 2020, we began to observe an increase in the third next available appointment (TNAA), in days, in the OPD. Our highest recorded TNAA during the period was 18 days (Figure 1). With continuous monitoring of the data points and validation, the TNAA remained above the target of <14 days. Given these data, we decided to address pressing issues that affect patient access to specialized services in the OPD.
Available Knowledge
Well-timed access to specialty care contributes to the improved health of patients.2 In order to improve efficiency and effectiveness, an institution needs to focus on two of the most important characteristics it must possess: availability and accessibility.3
The OPD at AHAFH provides specialized services to adult and pediatric patients, including but not limited to routine care, health promotion, disease prevention, and surgical services. Ease of accessibility to outpatient services has been shown to increase patient satisfaction and quality in delivering care to patients; however, with recent COVID-19 pandemic issues, it has been challenging for patients to access healthcare in general, which may be due to a shortage of physicians and nurses, and an increasing number of patients with chronic diseases. An efficient way to address accessibility issues is looking at the TNAA.
Poor coordination between referring physicians and specialists, lack of established referral criteria, and lack of appointment mapping coordinators for specialized services constitute the critical barriers to patients’ access to specialty care. A high TNAA indicates a backlogged system that may be due to poor access,4 delayed care for patients, increased number of no-shows, and increased number of walk-in patients. The reopening of the OPD demanded the pressing concern of delayed patient appointments due to increased volume and availability of resources be addressed.
Numerous studies are available describing challenges and methods to address issues related to access in outpatient departments. Through the MODHS in 2020, the project was initiated and proliferated to the armed forces hospitals throughout the kingdom with the aim to better understand the outpatient departments’ challenges on patient flow process, supply and demand, and the mechanism behind queuing. The MODHS provided training lectures and guidelines on implementing the initiative. Policies were also developed and communicated to all armed forces hospitals.
Specific Aim
The SMART (Specific, Measurable, Achievable, Relevant, and Time-Bound) aim statement of our quality improvement project is “To reduce the overall TNAA at the outpatient department specialty clinics of Al Hada Armed Forces Hospital from 14 days to 10 days by the end of Q1 2022.”
Specific- Reduce the third next available appointment at the Outpatient Department in AHAFH.
Measurable- The goal was to reduce the TNAA from 14 days to 10 days.
Achievable- The goal was feasible as it involved modest reduction of four days, considered achievable through an improvement process.
Relevant- The goal aligned with the hospital’s commitment to enhancing patient access, patient safety, and ensuring timely treatment and a better patient experience.
Time-Bound- The goal was set to be achieved by the end of Q1 2022, providing a definite time frame.
Rationale
The TNAA is a significant concept used in AHAFH in scheduling of appointments in the OPD. It denotes the third earliest appointment slot after the first available one, helping our physicians gauge the urgency of the patient’s condition. This method aids in efficient resource allocation, ensuring more urgent cases receive earlier attention while nonurgent cases are scheduled later.5,6
Observing and monitoring TNAA offers valuable insight on other alternative approaches, such as virtual clinics and phone consultations, not only to improve access, but also to enable physicians to streamline follow-up processes. A multivoting technique identified that the three main reasons affecting TNAA days are increased number of patient walk-ins, lack of referral criteria in specialties, and noncompliance with policies and procedures (Figure 1).
Context
The AHAFH OPD provides specialized tertiary level care with 40 specialties and subspecialties to both adult and pediatric clients, with 250,937 (about 20,911 per month) annual OPD visits. These OPD services cater to a wide range of healthcare needs, from routine checkups and preventive care to diagnostic tests and treatments for our patient population. The OPD services promote continuity of care by ensuring timely and appropriate care through providing accessible and comprehensive medical services to its patients.
Methods
Intervention
A team consisting of the medical director, OPD manager, head nurse and team leaders, information and communication technologies (ICT) staff, and a continuous quality improvement (CQI) and patient safety specialist was formed. The hospital director fully supported the initiative to address accessibility issues in the OPD. The team anticipated challenges in collection and validation of data due to the number of clinic specialized services (40 specialized services). A weekly administrative huddle was conducted to keep the team updated about the weekly data and project progress, as well as discuss issues concerning the challenges they faced. The nurse team leaders of each specialized service together with the head nurse also conducted daily huddles. We developed a calculation sheet to calculate the supply and demand capacity of the clinic specialties in the OPD (Figure 2). In order to address the clinic backlogs, we conducted a meeting with all stakeholders and heads of departments (HODs) to review the backlogs in their specialties. The HODs decided to have a mapping coordinator review referred cases to their specialty.
Considering that a high TNAA affects other indicators, we developed action plans to address no-show issues in OPD in collaboration with the ICT department, which include reminding patients about their appointment through text messaging and a call center in the OPD that informs and reminds patients a day prior to their appointment day. Educational materials were provided at the initial phase of the project to all patients to guide them on the changes made with the current process in the OPD.
Continuous monitoring is in place to ensure compliance from the stakeholders and end users. The Plan-Do-Study-Act (PDSA) model for improvement was utilized to implement action plans and interventions to address the increase of TNAA (in days) in the OPD (Table 1).
Study of the Intervention
To study the effect of multiple PDSA cycles in improving the TNAA to meet our target aim, we used pre-test and post-test quasi-experimental design. The study aims to evaluate the effectiveness of implementing PDSA cycles in optimizing scheduling processes, specifically focusing on the TNAA, in order to enhance patient access and reduce wait times.
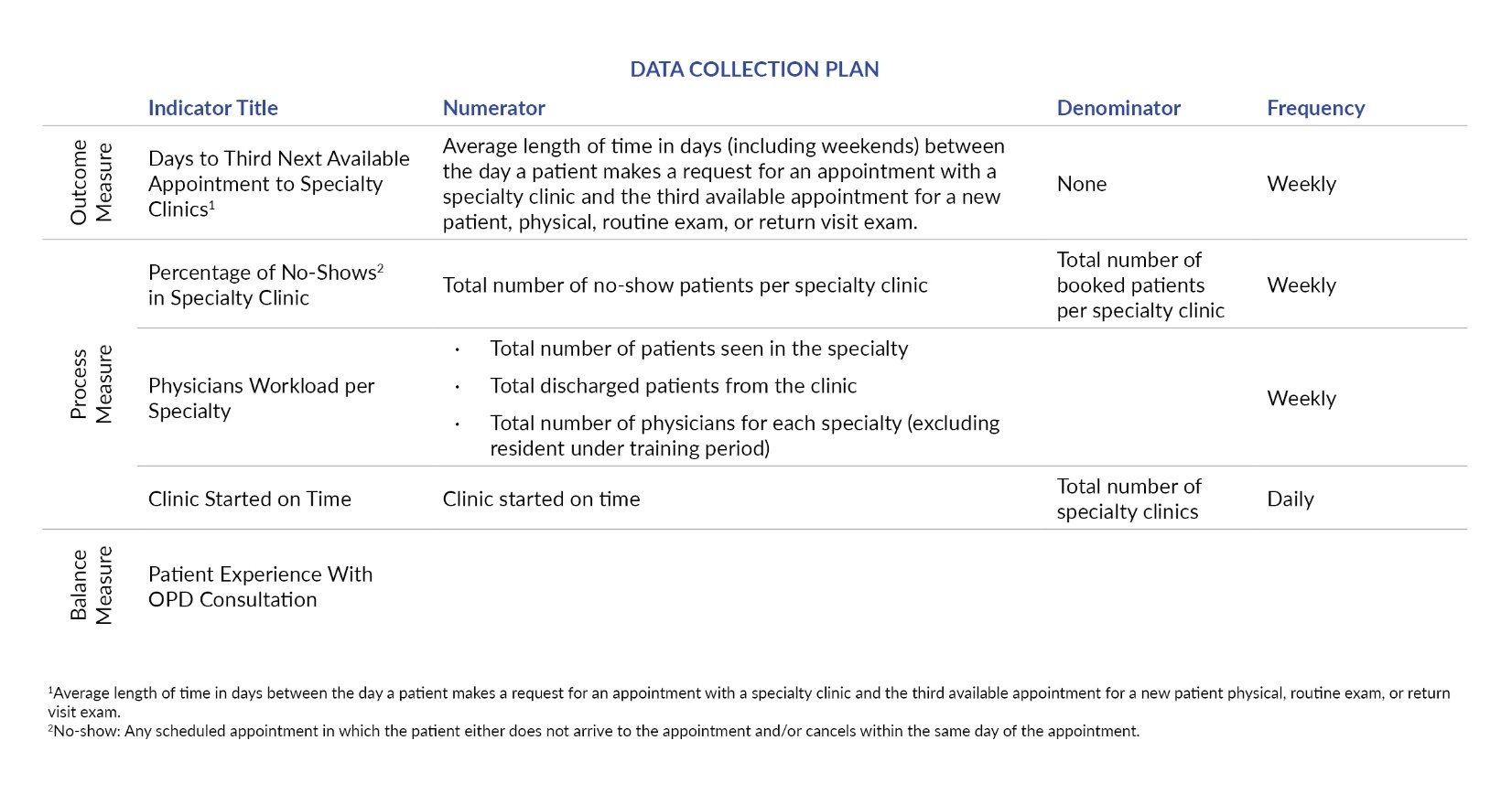
Measure
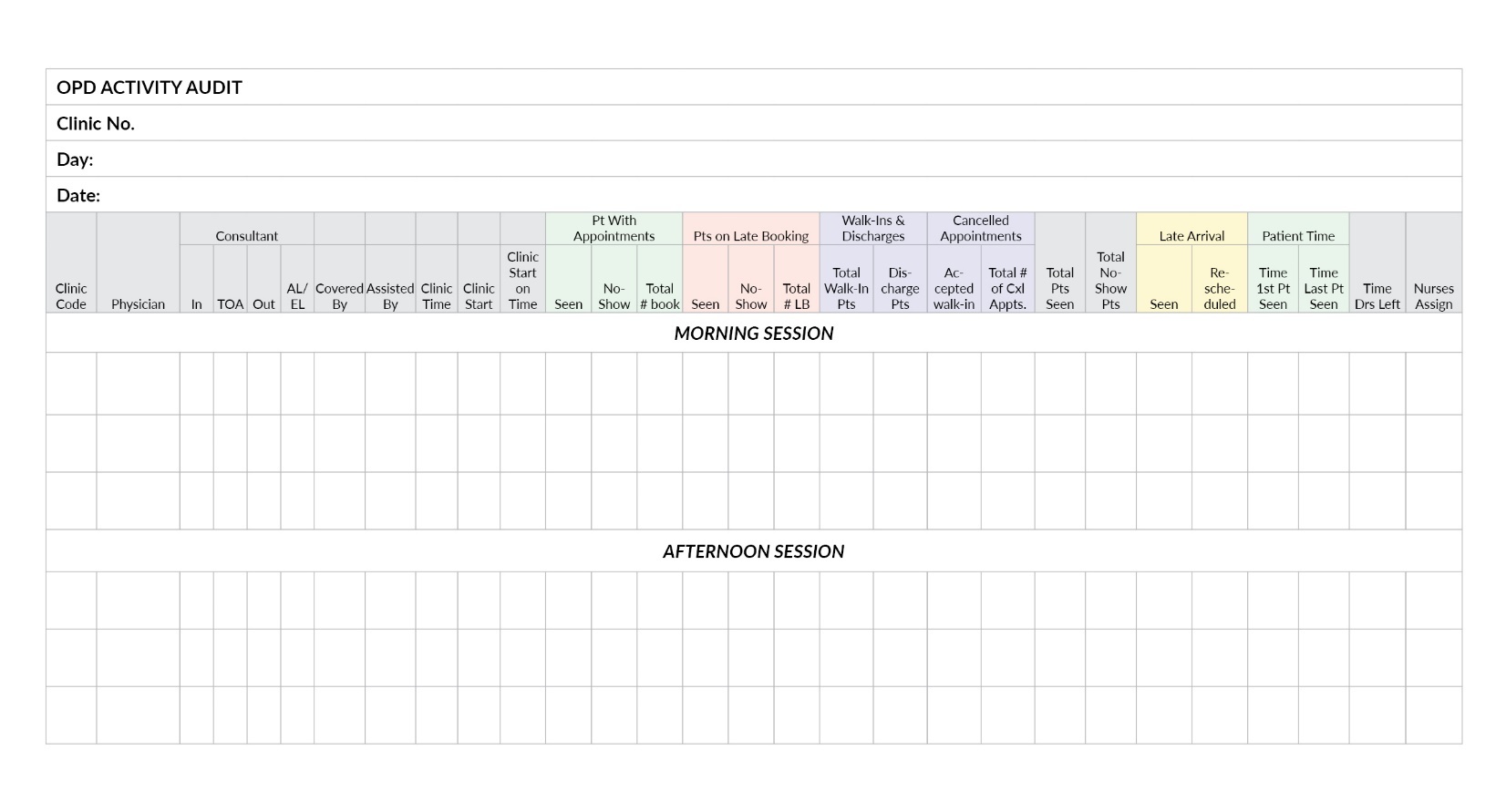
The initial data collection for this project focused on 40 specialties in the OPD to acquire a better understanding of the problem. Our data collection plan includes outcome measures, process measures, and balancing measures. Each indicator has a clear collection process including its numerator and denominator (Figure 3). A trained nurse in the OPD collects TNAA data every Monday and transcribes it to the TNAA data collection sheet. All other data are collected by the team leader of each clinic specialty, entered on the OPD data collection sheet (Figure 4), and submitted on Thursday afternoon after the last clinic session and the last patient seen. The data are then transcribed to the aggregation sheet (Figure 5) and manually validated by an assigned quality specialist.
Analysis
The data analysis was conducted using a control chart methodology. This allows visualization and interpretation of the collected data that enables a better understanding of the trends, patterns, and statistical variation during the course of the study. In order to assess the impact of the interventions, process measures and balancing measures were also analyzed. Evaluation of intervention on improving scheduling processes, reducing wait times, and enhancing access to care were part of the process measure analysis, while staff workload, patient satisfaction, and overall quality of care were included in the balancing measure analysis. The data were analyzed by using Microsoft Excel.
Data was collected using various sources, such as patient surveys, data collected by assigned team leader, and electronic health record in the Wipro system. These data were aggregated and analyzed to quantify the impact of interventions.
Results
The average TNAA (in days) in each quarter significantly decreased, with an average of 6 days in Q1 2022. During the intervention period, it can be seen in the control chart that there was a shift of mean, the upper control limit (UCL), and lower control limit (LCL). The post-intervention average TNAA (in days) remained within the target (<14 days). In Q4 2020 (before the intervention), the highest TNAA recorded was 18 days. Although there was a decrease in TNAA in the last week of the quarter, there was no sustainability. Upon implementation of the first PDSA cycle in Q1 2021, there was no significant improvement on the data, and the highest data point recorded was 17 days. The second PDSA cycle was implemented in Q2 2021 and although there were recorded TNAA days within and below the 14 days target, we agreed that there was no sustainable gain during the period.
During this period, we also ensured the accuracy of data by checking the collection process of team leaders and manual validation by the CQI staff. In the third PDSA cycle, in which we implemented reminder messages to patients to address the no-show and strategic optimization, we observed a significant decrease in TNAA. This success is attributed to implementation of the PDSA cycle and continuous monitoring of the previously implemented plans. The TNAA has continuously decreased with the fourth PDSA cycle and remained below the established target of <14 days, as shown in the control chart (Figure 6).
Pre-intervention mean TNAA was 9.4 days compared to the post-intervention TNAA of 5.6 days (a decrease of 3.8 days).
Discussion
Summary
Standardizing the referral system and referral type,1 monitoring the supply and demand of the clinics,4 and sending reminder messages to patients can result in an improvement of TNAA, thereby improving the quality of care in outpatient clinics. Our project also highlights the complexity of the efforts required for continuously improving the TNAA at busy outpatient settings.
A key lesson learned during the project period is the importance of leadership involvement. Their buy-in is crucial to produce change and set direction to cope with change. Leadership will motivate and guide people to realize the potential and address tougher challenges along the way. One of the major reasons why a project fails is lack of communication. Keeping stakeholders and end users involved, updated, and informed is one of the vital points to build trust and gain their cooperation.
Another essential learning that took place during the project period is using the right quality tool. While many tools can be used during a project, it is crucial to identify the right tool that applies to the project. We utilized the PDSA cycle model, which allowed us to implement our action plan in a step-by-step method and gave us the opportunity to look back and reevaluate action plans that were not effective.
Interpretation
There was a decrease in TNAA in days, which indicated a significant decrease in patient wait time for appointments, thereby improving patient access in the outpatient setting. Implementation of the PDSA cycles led to a positive change in the service provided by the OPD, which in turn enhances patient access and satisfaction. While the pandemic introduced complexities in providing care and disruption and constraint in services provided by AHAFH, addressing these issues through the scientific method ensures efficient patient flow while maintaining patient safety.
Our intervention at AHAFH aligns with the successful strategies employed by a healthcare facility in Doha, Qatar. Both healthcare facilities undertook projects aimed at reducing the third next available appointment in the outpatient department through streamlining appointment scheduling and enhancing patient flow management.
Strengths and Limitations
One of the strengths of this project is the use of a well-established quality improvement methodology, the PDSA tool. Focusing on the specific measure on TNAA provided us with a clear, measurable outcome for evaluating the effectiveness of the interventions.
Our project highlighted barriers related to staffing, specifically with nursing. Nurses play an integral part in the implementation of the action plans developed. Putting this into consideration, we coordinated with the OPD head nurse and the Nursing Department and they were able to develop a comprehensive optimization plan for the OPD. Technology plays a major role in moving forward with the improvement project; however, the use of a third-party company for the hospital information system also plays a major role in one of the project’s setbacks, due to the need to contact the company to make changes or adjustments to conform with the agreed action plans.
One project limitation is that our project is the work of a single healthcare institution department at the local emergency department, which could limit generalizability. However, we believe that the basic principles described in using an organizational values-aligned behavioral model and evaluating its effectiveness, using the Institute for Healthcare Improvement model for improvement PDSA, could be easily extrapolated to other types of institutions.
Conclusions
At the start of PDSA cycle 3 in Q3 2021, we started to notice a decrease in TNAA, with an average of 7 days. It continued to stay below the target (<14 days) in Q4 2021 (average of 3 days) and Q1 2022 (average of 6 days).
The success in reducing the TNAA predicated on three key points:
a) We approached quality improvement methodically, utilizing structured quality tools, such as Ishikawa diagrams, and measuring our outcome with a run chart or control chart.
b) We identified our critical path and addressed it with PDSA cycles, which proved to be an effective method in this project.
c) The standardization of the process in all clinics’ specialized services helped maximize efficiency in practice and improve accessibility to the OPD.
By modifying the current practice, revising the policies and procedures, and involving stakeholders in every step of the quality improvement project, we allowed the physicians and nurses to provide efficient and effective care to our patients. Our next step is to sustain our success by continuously monitoring the indicators and dissemination of findings and action plans to all stakeholders.
Ethical Consideration
The quality improvement project did not require organizational ethics committee approval.
Acknowledgement
We would like to acknowledge the executive leadership and Col. Baker Al Johani, MD, for unwavering support on this project. We would like to acknowledge the contributions of all Al Hada Armed Forces Hospital Outpatient Department staff, nurses, and leadership. Their continuous effort to improve outpatient services and patient safety is commendable. This project would not be possible without them.
Author Contributions
RSB: Writing-Original Draft, Writing-Review & Editing, Data Curation, Methodology, Formal Analysis, Investigation, Resources. MHA: Writing-Review & Editing, Formal Analysis, Resources. LE: Project Administration, Methodology, Formal Analysis, Resources. ASA: Project Administration, Resources. MDV: Data Collection, Methodology. JDA: Methodology, Resources. JAN: Conceptualization, Project Administration, Resources.
Disclosure
The authors declare that they have no relevant or material financial interests.
About the Authors
Reynan Subahani Bautista (bautistascfhs87@gmail.com) is a registered nurse and a Continuous Quality Improvement and Patient Safety workforce member. He earned his Bachelor of Science in nursing in 2007 at Western Mindanao State University. Currently, he is pursuing a master’s degree in nursing with specialization in nursing administration at the Philippine Women’s University.
Muhammad Hasan Abid is the regional head of Patient Experience & Continuous Quality Improvement and patient safety specialist at the Armed Forces Hospitals Taif Region (AFHTR). He is also an Institute for Healthcare Improvement Fellow and Mentor. He provides leadership and strategic alignment of the quality improvement and patient safety projects with the strategic goals for patient experience at the AFHTR.
Lamiaa Elmasry is the head of the Quality Improvement Division at Al Hada Armed Forces Hospital in Taif Region, Saudi Arabia. She is in the medical profession with a total quality management diploma and hospital management diploma from the American University in Cairo. Additionally, Dr. Elmasry has Lean Six Sigma Green and Lean Specialized qualification from ASQ (American Society for Quality). Moreover, she is an improvement advisor candidate at the Institute for Healthcare Improvement.
Abdulaziz Saleh Alamalki is currently a physician at Al Hada Armed Forces Hospital and the head of the Medical Violation Department. He was the Outpatient Department Director from 2020–2021. He was part of the Healthcare Quality Management Program by the Ministry of Defense for Health Services in 2022.
Marynette De Vera is the Outpatient Department head nurse at Al Hada Armed Forces Hospital. She earned her Master of Science in nursing degree at University of La Salette in the Philippines.
Jean Barrientos De Asis is a registered nurse specializing in emergency nursing and a Continuous Quality Improvement and Patient Safety workforce member. She earned her Master of Arts in nursing in 2015 at Urdaneta City University in the Philippines. She is a certified professional in healthcare quality and a certified Lean Six Sigma Master Black Belt and has worked in several improvement projects at Al Hada Armed Forces Hospital.
Jamal Al Nofeye is the regional director of Continuous Quality Improvement and Patient Safety in Taif Region, Saudi Arabia. He is a current board member of the Taif Health Cluster. He is a physician with double master Executive Master of Business Administration (Hon) Master of Healthcare Quality and Safety (Harvard Medical School) and a certified project manager.







_with_mean_score_variation_and.jpeg)





_with_mean_score_variation_and.jpeg)