Introduction
Problem Description
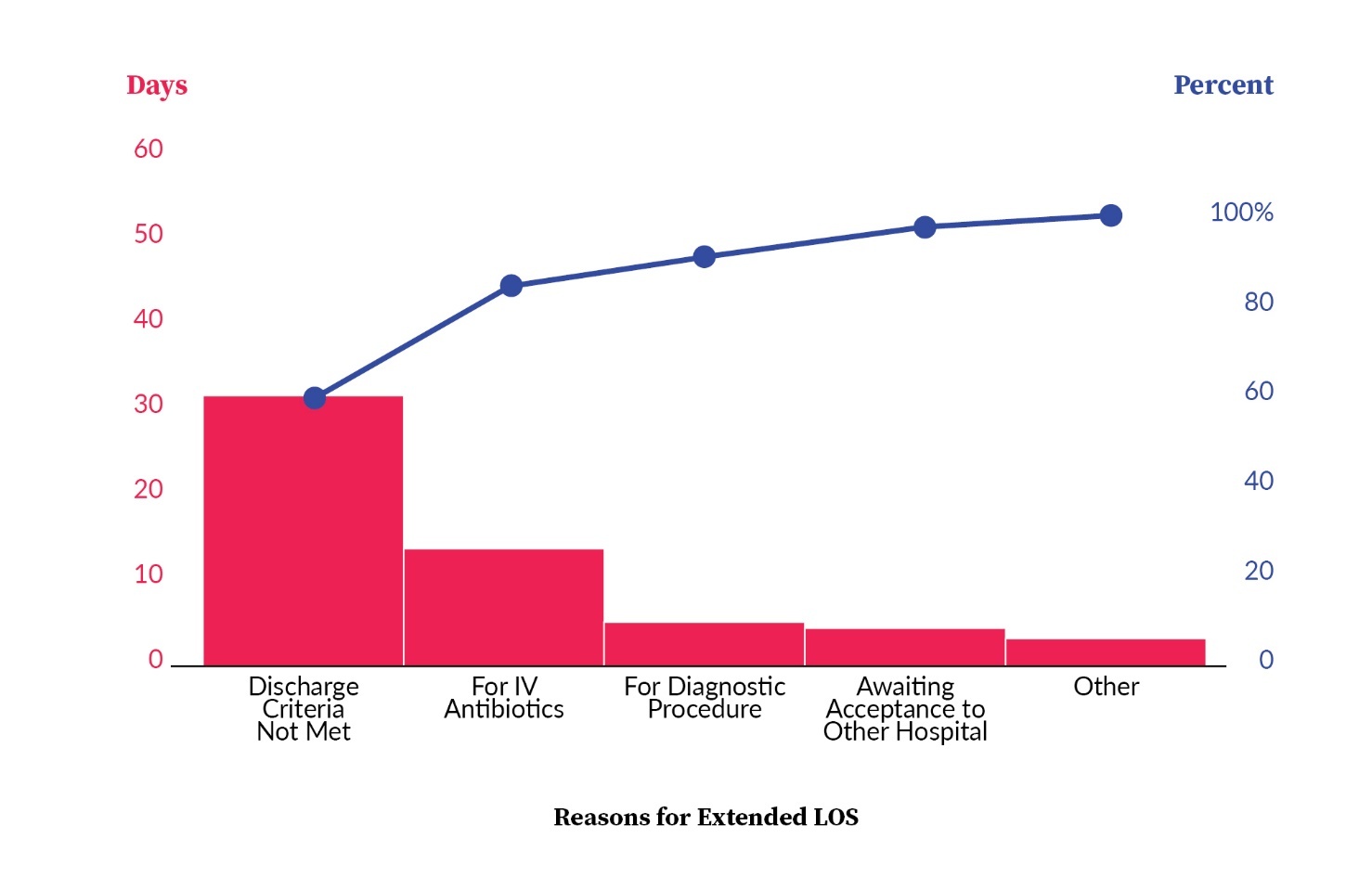
The challenge of extended hospital stays exceeding seven days at Al Hada Armed Forces Hospital (AHAFH), often due to patients needing to complete intravenous antibiotic treatment, prompted a critical intervention. This issue came to the forefront in October 2020 when approximately 23% of patients with length of stay beyond seven days were receiving antibiotics only. The solution was to establish outpatient parenteral antimicrobial therapy (OPAT) clinics, with a primary focus on ensuring patient safety throughout the transition.
Available Knowledge
A substantial body of prior research has provided compelling insights into the practice of OPAT. OPAT is defined as the administration of ≥2 doses intravenous antimicrobials outside an acute care setting.1 OPAT falls under the umbrella term “complex outpatient antimicrobial therapy” (COpAT), which includes both oral and intravenous antimicrobials given for a prolonged period and usually requiring outpatient monitoring.2
The practice of OPAT and COpAT has been expanding in recent years. OPAT has become more common in clinical settings. In recent years, there has been a notable shift in Saudi Arabia towards prioritizing ambulatory and outpatient healthcare services for conditions traditionally treated in hospitals.3 This change is predominantly driven by factors such as healthcare cost considerations, patient preferences, and an increased awareness of hospital-acquired infections.4
OPAT, introduced by Rucker and Harrison in 1974, has evolved into an approved outpatient healthcare service.5,6 It offers advantages over traditional approaches, enabling patients to recover at home, enhancing overall satisfaction.7 A recent study by Yadav et al. highlighted OPAT’s positive impact, reducing emergency department visits and therapy failure rates.8
Moreover, OPAT minimizes the risk of nosocomial infections and proves cost-effective for healthcare facilities, optimizing resource use and bed occupancy.9–11 The program offers two implementation models: an OPAT infusion clinic (IC-OPAT) and an OPAT home infusion service (H-OPAT).11
The OPAT program was launched at AHAFH in November 2020, marking its initial implementation. This program aimed to achieve several key objectives. Firstly, it sought to establish a standardized process for the administration of parenteral antimicrobial medications in an outpatient setting, catering to patients requiring prolonged antimicrobial therapy. Secondly, the program aimed to ensure the safe and effective delivery of parenteral antimicrobial treatments within a community-based healthcare environment. Another significant goal was to contribute to the reduction of microbial resistance within the healthcare system. Furthermore, the program played a role in evaluating patients who had been discharged from other hospitals but still required parenteral antimicrobial therapy. Additionally, it aimed to reduce the length of hospital stays and lower the overall cost of healthcare services. Lastly, the implementation of a bed management system was part of the effort to enhance bed turnover efficiency within the hospital setting.11
Rationale
The rationale behind the introduction of OPAT is firmly rooted in established healthcare frameworks, models, concepts, and theories that have shaped the field of healthcare delivery. These components collectively provide a robust underpinning for comprehending the issue at hand and devising the OPAT intervention. Infectious disease management frameworks emphasize the urgency of timely and effective treatment, a principle that OPAT addresses by transitioning patients to outpatient settings while upholding safety and compliance. Transitional care models endorse the idea of seamless shifts between different levels of care, a core tenet of OPAT’s success. Patient-centered care concepts underscore the importance of patient preferences and their active participation in treatment decisions, a principle embodied by OPAT, which grants patients the option of receiving care in their homes or outpatient settings. Moreover, OPAT aligns with antibiotic stewardship principles, focused on the responsible use of antibiotics, which leads to optimized treatment regimens and a reduction in healthcare-associated infections.
Economic models provide added support for OPAT’s rationale by demonstrating cost savings achieved through diminished hospitalization costs without sacrificing care quality. Furthermore, OPAT interventions may address concerns related to environmental sustainability by promoting the use of more environmentally friendly oral antibiotics. This multifaceted rationale underscores that OPAT is grounded in healthcare best practices, patient-centered care, antibiotic stewardship, cost-effectiveness, and environmental responsibility, with the expectation that it will effectively address the issue of prolonged hospital stays linked to intravenous antibiotics.
Aim
Primary Aim
Specific: The primary objective was to reduce the number of hospital bed days associated with long-term antibiotic therapy, with a focus on a 20% reduction.
Measurable: The goal was to achieve a 20% reduction in bed days within the first year, from November 2020 to October 2021, equivalent to 200 fewer bed days compared to the baseline of 986 bed days.
Achievable: This goal was deemed attainable through the implementation of strategies that enhance resource efficiency and patient flow.
Relevant: The initiative aligns with the objective of optimizing resource utilization and patient care within the healthcare facility.
Time-bound: The target was to achieve the 20% reduction within the first year, specifically by the end of October 2021.
The principal objective of this initiative was to achieve a substantial reduction in the number of hospital bed days attributed to patients requiring long-term antibiotic therapy. Specifically, the project targeted a reduction of 20% within the first year of implementation, spanning from November 2020 to October 2021. This reduction goal translates to a noteworthy decrease of 200 bed days when compared to the baseline figure of 986 bed days. The primary aim underscores the project’s commitment to enhancing resource efficiency and patient flow within the healthcare facility.
Secondary Aim
Specific: The secondary objective was to reduce the percentage of patients with a hospital stay exceeding seven days for antibiotic treatment.
Measurable: The goal was to decrease the percentage from 23% (baseline) to 15% within a year from the project’s start in October 2020 to October 2021.
Achievable: This target was deemed attainable through improved healthcare practices and patient management.
Relevant: The objective aligns with the project’s focus on enhancing patient care, safety, and healthcare efficiency.
Time-bound: The aim was to achieve a reduction in the percentage by October 2021, marking one year from the project’s commencement in October 2020.
In addition to the primary goal, the project also had a secondary aim, which focused on improving patient care. The secondary objective aimed to reduce the percentage of patients exceeding a seven-day hospital stay to receive antibiotics. Prior to the project’s commencement, this figure stood at 23%. Over the course of a year from the project kickoff in October 2020, the aim was to bring this percentage down to 15% by October 2021. This secondary aim emphasizes the project’s dedication to enhancing patient safety, quality of care, and overall healthcare efficiency.
Context
Expanding on the contextual elements considered during the introduction of the OPAT intervention is essential to appreciate their significance fully. Patient population assessment goes beyond identifying the types of infections, extending to understanding the clinical profiles of patients who can benefit from OPAT. This knowledge informs the development of tailored treatment plans and criteria for patient eligibility, ensuring that OPAT is administered to those who will benefit the most.
In addition to patient-specific considerations, the establishment and adherence to clinical guidelines and protocols are pivotal in promoting the standardization of care, which is essential in healthcare delivery. This not only streamlines the OPAT process, but also assures patient safety by ensuring consistent and evidence-based treatment. Standardized protocols help healthcare providers make informed decisions, reduce variability in practice, and enhance overall treatment efficiency. Moreover, a standardized approach facilitates communication among healthcare professionals, fostering a collaborative and cohesive environment for the successful implementation of OPAT interventions.
A robust healthcare infrastructure, including outpatient clinics, home healthcare services, and support from outpatient pharmacies, provides the necessary logistical backbone for OPAT. Having these elements in place ensures the safe and efficient delivery of care in nonhospital settings, allowing patients to receive their treatment with ease.
The interconnectedness of these components forms a comprehensive ecosystem that not only addresses the medical aspects of OPAT, but also considers the practical and logistical aspects, ultimately contributing to the success and sustainability of outpatient antimicrobial therapy initiatives. This holistic approach ensures that OPAT is not just a medical intervention but a well-integrated and coordinated healthcare strategy aimed at optimizing patient outcomes and improving the overall efficiency of outpatient antimicrobial treatment.
Staffing and training stand as pivotal components in ensuring that healthcare professionals are well prepared to manage OPAT effectively. Adequate training in the administration of OPAT, patient monitoring, and communication among the care team are essential to maintain the safety and quality of care. Healthcare providers involved in OPAT should receive comprehensive education on the specific protocols, procedures, and best practices associated with outpatient antimicrobial therapy. This training not only equips them with the necessary clinical skills, but also fosters a deeper understanding of the unique challenges and considerations involved in providing care outside the traditional hospital setting.
Moreover, staffing levels need to be carefully assessed and adjusted to meet the demands of OPAT, ensuring that there is a sufficient number of trained professionals to deliver care efficiently. This includes not only nurses and physicians, but also pharmacists and other allied healthcare professionals who play crucial roles in the success of OPAT initiatives. Adequate staffing ensures that patients receive timely and appropriate interventions, that monitoring is thorough, and that potential complications are addressed promptly.
Patient education and obtaining informed consent cannot be overstated. Patients need to be fully informed about the nature of OPAT, its potential benefits, and any associated risks. This not only empowers patients to make informed decisions, but also contributes to their active engagement in the treatment process, which is often a key driver of positive outcomes. In the process of patient education, healthcare providers should communicate clearly and effectively, using accessible language to ensure that patients understand the rationale behind OPAT, the medications involved, and the importance of adherence to the treatment plan.
In addition to the potential benefits and risks, patients should also be educated about the proper administration of medications, potential side effects to monitor, and steps to take in case of any concerns or complications. Clear communication about follow-up appointments, monitoring requirements, and contact information for healthcare providers is crucial to establish a collaborative and supportive patient-provider relationship.
Obtaining informed consent is an ethical imperative in OPAT. It ensures that patients are aware of the treatment plan, potential risks, and alternatives, and willingly agree to participate. The process of obtaining informed consent should be transparent, allowing patients the opportunity to ask questions and seek clarification on any aspect of OPAT. This not only protects the rights and autonomy of patients, but also fosters trust between healthcare providers and patients, laying the foundation for a successful and cooperative therapeutic relationship throughout the OPAT journey.
Understanding the financial implications of OPAT is vital, as it can influence reimbursement models, budget allocations, and overall cost-effectiveness. Evaluating the economic impact of OPAT and quantifying potential cost savings are essential to justify its implementation. Healthcare institutions and policymakers need to conduct thorough analyses that consider not only the direct costs of outpatient antimicrobial therapy, such as medication and administration expenses, but also the indirect costs associated with potential complications, hospital readmissions, and the overall impact on healthcare resources.
Furthermore, assessing the cost-effectiveness of OPAT involves comparing it to traditional inpatient care models, taking into account factors like length of hospital stay, resource utilization, and associated healthcare expenditures. By demonstrating the economic benefits of OPAT, healthcare systems can make informed decisions about resource allocation and reimbursement structures, ultimately optimizing the allocation of funds and ensuring the sustainability of OPAT programs.
Outcome measurement and quality metrics must be defined from the outset to gauge the success of OPAT. These metrics can encompass clinical outcomes, patient satisfaction, and cost-effectiveness, providing a comprehensive assessment of the intervention’s impact.
Finally, fostering collaboration and an interdisciplinary approach among various healthcare professionals and services is essential for the coordinated care of patients undergoing OPAT. Effective communication and shared responsibilities ensure that patients receive comprehensive care in a seamless and efficient manner.
In sum, these contextual elements collectively define the landscape in which OPAT operates. Their thoughtful consideration and integration are vital in ensuring the successful introduction of OPAT, resulting in safe, quality care and cost-effective healthcare delivery.
Methods
Interventions
The leadership and operation of the OPAT service at AHAFH are primarily overseen by Infectious Disease physicians, who extend their expertise to both the pediatric and adult patient populations. Patients are assessed for eligibility based on approved OPAT inclusion and exclusion criteria. The delivery of OPAT takes place in a designated OPAT infusion unit situated within the emergency department (ED), where patients attend as outpatients daily or twice a day until the prescribed intravenous antibiotic regimen is completed.
To drive a quality improvement initiative in OPAT, a project team was assembled, comprising key individuals such as the assistant hospital director for Health Affairs (the project sponsor), the medical director (the project owner), and other vital stakeholders. This interdisciplinary team includes the Infectious Disease chairman, physician champion, nurse champion, ED physicians and nurses (OPAT clinic), clinical pharmacist, bed manager, quality improvement coach, and other staff members. The development of a comprehensive policy involved the input and collaboration of these key stakeholders.
Within this framework, the Infectious Disease physicians hold the responsibility of evaluating patients for OPAT suitability, prescribing the appropriate intravenous antimicrobial regimen, and formulating a treatment plan. When OPAT is deemed suitable, the patient, or their family, is engaged in a discussion regarding the intravenous (IV) line. For patients with an anticipated IV antibiotic course of less than seven days, a peripheral IV catheter is inserted on the first day of the OPAT treatment. In cases requiring IV antimicrobial therapy exceeding seven days, arrangements are made for the insertion of a long-term IV catheter through interventional radiology. The initial responsibility for monitoring adverse events or medical complications that may arise during the therapy falls to the ED physician, who subsequently refers the patient to their primary physician. Communication between the OPAT nurse and the primary physician is vital for addressing medical issues and concerns. Additionally, the primary physician is informed once parenteral treatment is either completed or missed.
During the implementation of the OPAT project, one significant challenge encountered was physician resistance to discharging patients to OPAT. To mitigate this risk, a strategy of continuous education, leader engagement, and the appointment of physician and nursing champions was employed. Another concern during project planning was the geographical location of AHAFH and patient commitment to attend the OPAT clinic daily.
The improvement methodology adopted for this project is the Plan-Do-Study-Act (PDSA) cycle. This systematic approach enables the team to measure the impact of changes and ascertain the effectiveness of interventions. The implementation team maintains regular meetings throughout the project to monitor OPAT’s progress. Furthermore, providers and staff receive comprehensive education on the OPAT policy, procedures, and required documentation. New providers and staff receive orientation led by the nurse and physician champions.
The team is devoted to ensuring the safety of patients in the OPAT clinic, with a primary focus on a detailed review of the inclusion and exclusion criteria to ensure that only appropriate patients receive OPAT treatment. This comprehensive approach highlights the hospital’s commitment to delivering effective and safe OPAT services.
Study of the Interventions
The chosen approach for assessing the impact of the OPAT intervention at AHAFH involves a comprehensive and systematic evaluation process. The primary methodology employed for this assessment is the PDSA cycle, which allows for iterative testing, measurement, and improvement.
PDSA Cycle 1
During the initial PDSA cycle, the central goal was to lay the groundwork for the OPAT program within the institution, encompassing the establishment of both the necessary infrastructure and the associated operational procedures. This involved crucial steps, such as crafting a comprehensive hospitalwide policy and procedure for OPAT that included specific criteria for patient inclusion and exclusion. The resulting policy was submitted to the medical administration for implementation. To ensure a well-prepared staff, healthcare providers (including physicians, nurses, and pharmacists) received orientation and training about the new OPAT service. The allocation of five emergency room beds by the hospital administration to serve as the OPAT unit was a pivotal development, providing the physical infrastructure for the program’s delivery. Monitoring and evaluation of the program’s progress, with a focus on the number of enrolled OPAT patients, was a regular agenda item during daily meetings.
However, the study phase of this initial PDSA cycle yielded essential insights. It became evident that the project in its current form was not sustainable. Enrollment was quite limited, with only one patient in November 2020 and another in December 2020. This low enrollment was attributed to stringent inclusion criteria that restricted eligibility to patients requiring once-daily antibiotic therapy. The impact of the COVID-19 pandemic, coupled with the implementation of lockdown measures, further contributed to the challenges faced during this phase.
These findings underscored the need for adaptability in the OPAT program to make it more accessible to a broader patient population. Future PDSA cycles are likely to center on adjustments that enhance the program’s sustainability, flexibility, and responsiveness to evolving patient needs and external factors like the pandemic.
PDSA Cycle 2
In the second PDSA cycle, the focus was on optimizing the OPAT program to better accommodate a larger number of patients. To achieve this, several significant changes were implemented, with the effective date being February 2021. First and foremost, the inclusion criteria for OPAT were revised, specifically regarding antibiotic frequency, which was adjusted from once daily to twice daily. This change expanded the eligibility criteria, making the OPAT service available to a broader spectrum of patients.
Moreover, the operational hours of the OPAT program were extended to provide service around-the-clock, seven days a week, departing from the previous 8 a.m. to 4 p.m. schedule. This extension was instrumental in offering patients greater flexibility and accessibility to OPAT treatment, ensuring that they could receive care when it best suited their needs. Recognizing that transportation challenges could hinder some patients from accessing the hospital for their OPAT treatment, a transportation service was introduced. Patients facing difficulties with traveling to and from the hospital were offered transportation support to overcome these barriers.
The key learnings from this cycle are multifaceted. Firstly, the importance of flexibility in inclusion criteria emerged, demonstrating that adaptability is crucial to accommodating a wider range of patients and their specific needs. Secondly, the cycle highlighted the significant impact of improved access to healthcare services, emphasizing the value of extended operational hours and enhanced transportation support in ensuring that patients can readily access OPAT. The cycle underscored the importance of regular monitoring and evaluation to assess program performance and make timely adjustments. Additionally, it reinforced the principles of patient-centered care, as the changes were aimed at addressing individual patient requirements and improving the overall patient experience. Lastly, the allocation of resources, such as transportation support, was shown to have a substantial impact on program effectiveness, highlighting the significance of resource allocation to overcome patient barriers and enhance the success and sustainability of the OPAT program. These key learnings reflect a commitment to ongoing improvement, adaptability, and the responsive tailoring of healthcare services to meet the evolving needs of the patient population.
PDSA Cycle 3
In the third PDSA cycle, we introduced a hypothesis aimed at optimizing the intervention’s efficacy. The hypothesis posited that conducting educational sessions about OPAT for physicians during their daily morning meetings could potentially yield better results. These sessions would specifically concentrate on elucidating the OPAT pathway and underscore the project’s advantages across diverse medical specialties, with the overarching objective of heightening awareness about the OPAT project. This educational strategy was implemented during the period from March to May 2021.
PDSA Cycle 4
In the fourth PDSA cycle, efforts were directed towards increasing physician engagement and encouraging them to refer patients to the Infectious Disease Department. To facilitate this, a physician champion was designated for each medical specialization. Their role encompassed overseeing patient flow and justifying extended length of stay (LOS) for patients who were unable to be discharged promptly. This justification was presented during the morning huddle with the Patient Flow Steering Committee. Furthermore, a streamlined process was established to refer patients who only required IV antibiotics to the on-call Infectious Disease team for assessment, with the goal of potential enrollment in the OPAT program. These adjustments, including the appointment of physician champions, were officially implemented in June 2021.
Measures
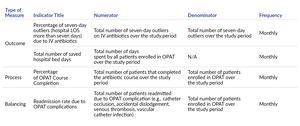
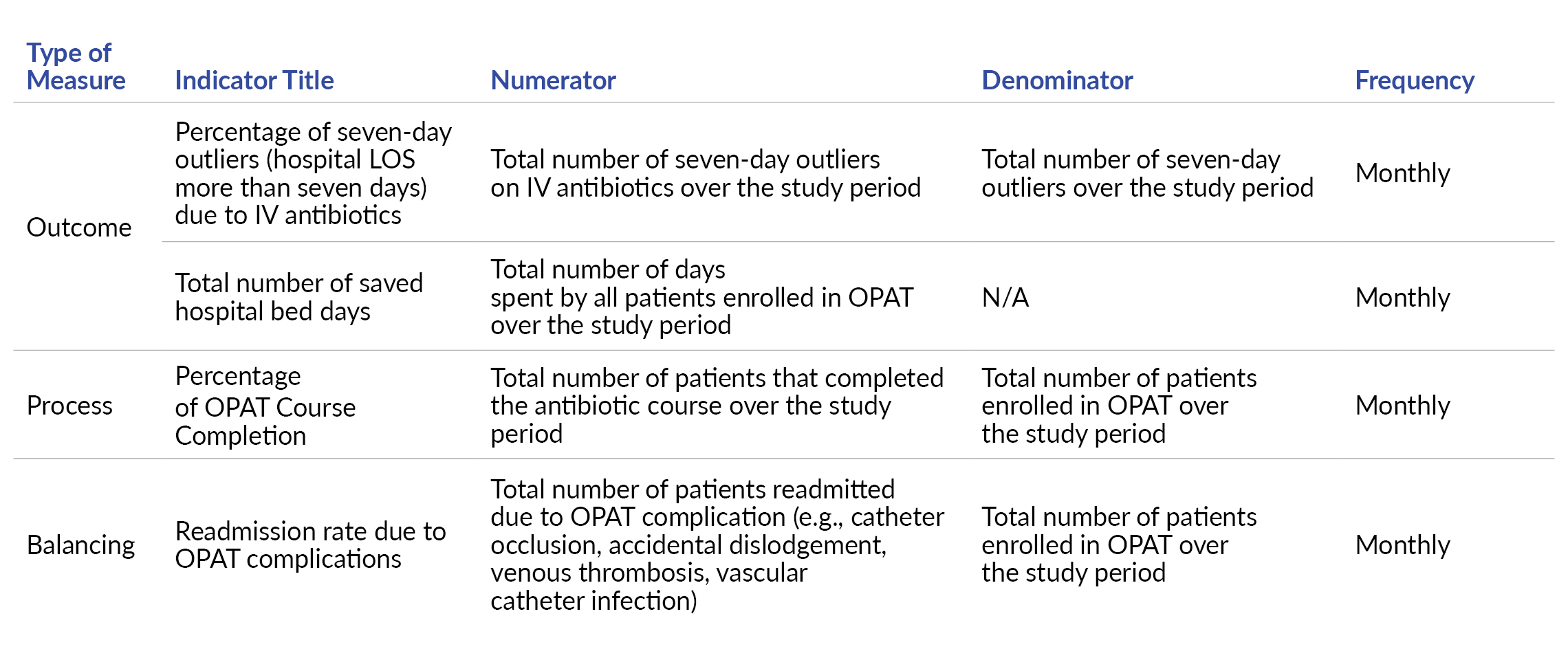
The key performance indicators (KPIs) employed in this project encompass outcome, process, and balancing measures to comprehensively assess the impact of the OPAT intervention. These KPIs are essential for evaluating both the quality and cost-effectiveness of the program.
The outcome measures in the project are twofold:
Percentage of Seven-Day Outliers Due to IV Antibiotics: This measure helps assess the extent to which OPAT has contributed to reducing the number of patients exceeding a seven-day hospital stay due to IV antibiotic therapy. It provides insights into the impact of OPAT on the length of hospital stays.
Total Number of Hospital Days Saved: This metric quantifies the cumulative number of hospital days saved as a direct result of patients receiving antibiotics through the OPAT program. It provides a tangible measure of the economic impact on the hospital, demonstrating potential cost savings.
While tracking outcome measures is crucial, it’s not the sole determinant of success in healthcare interventions. Therefore, process measures play a pivotal role in assessing the effectiveness of the care process and identifying areas of variation that could influence outcomes. The specific process measure used in this project is the “Percentage of OPAT Patients Who Completed the Antibiotic Course.” This measure evaluates the adherence and successful completion of the prescribed antibiotic regimen by OPAT patients. It serves as an important indicator of the effectiveness and reliability of the OPAT treatment process.
To ensure a balanced evaluation of the OPAT program, a balancing measure is also employed:
Readmission Rate Due to OPAT Complications: This measure assesses the rate of patient readmissions specifically attributed to complications related to the OPAT program. It helps in monitoring the safety and effectiveness of the OPAT interventions and provides insights into any potential adverse effects.
The inclusion of these outcome, process, and balancing measures creates a comprehensive framework for evaluating the OPAT program’s impact on patient outcomes, cost-effectiveness, and safety. It enables a well-rounded assessment of the quality of care and informs any necessary adjustments to enhance the program’s performance and patient outcomes.
Analysis
To ensure the accuracy and quality of data for informed decision-making, a robust data validation process was implemented initially and subsequently conducted on a monthly basis. This validation process involved a thorough review of patient medical record files, encompassing key elements such as physician referrals to the Infectious Disease Department, adherence to the inclusion and exclusion criteria, and patient attendance to the OPAT course.
The initial phase of the study focused on gathering baseline data, providing a comprehensive understanding of the existing conditions related to the outcome variable—such as hospital bed days for patients receiving long-term antibiotics and the percentage of patients exceeding a seven-day hospital stay for antibiotic administration. Subsequently, the OPAT intervention was introduced, and post-intervention data was collected to evaluate any changes in the outcomes.
The quasi-experimental design allows for a practical assessment of the OPAT intervention’s effectiveness in a real-world setting, considering the complex and dynamic nature of outpatient care. While random assignment is not employed, statistical methods are utilized to control for potential confounding variables, enhancing the reliability and validity of the findings. The comparison of pre- and post-period data is crucial for understanding whether the observed changes in outcomes, such as the considerable and sustained reduction in the number of stranded patients requiring IV antibiotics, can be attributed to the OPAT intervention. However, it’s essential to acknowledge that, in the absence of randomization, careful consideration of alternative explanations is required when making causal inferences. The quasi-experimental design serves as a pragmatic and ethical approach to assess the impact of the OPAT intervention, providing valuable insights for the ongoing improvement of outpatient antimicrobial therapy initiatives.
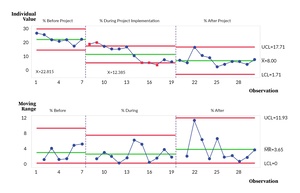
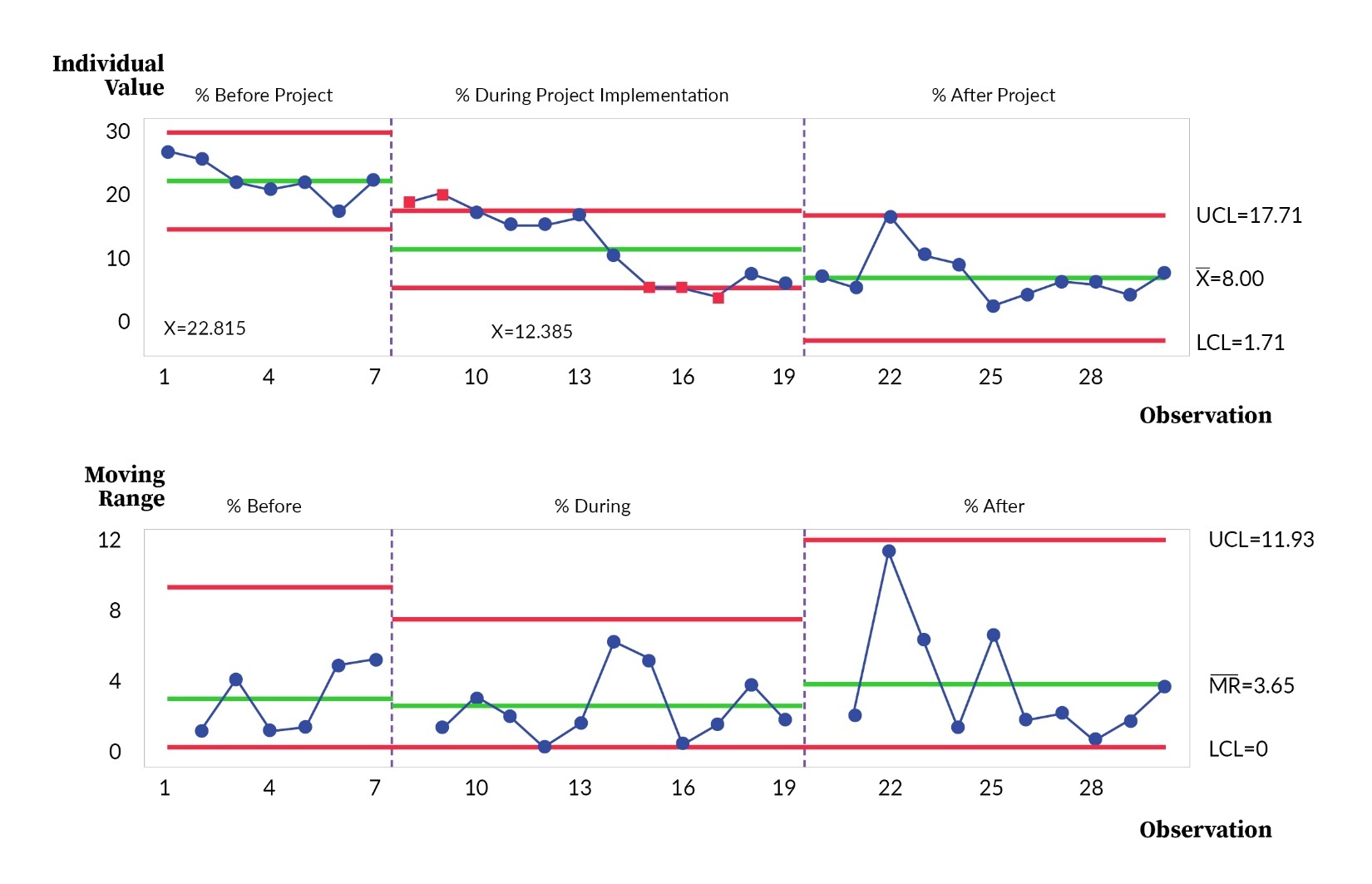
The descriptive statistics for the outcome, process, and balancing measures are provided as proportions and numbers. The percentage of seven-day outliers due to IV antibiotics (outcome measure) collected over time was reported as a control chart with pre- and post-intervention phase analysis.12 The corresponding mean, upper control limit (UCL), and lower control limit (LCL) were reported to identify improvements in this measure. Control chart was used to present the inferential statistics for the outcome measure to demonstrate the impact of the interventions and PDSA cycles over time. Statistical process control chart rules for the I-MR chart were applied to demonstrate special cause variations. Additional quantitative measures, encompassing both process and balancing metrics, were collected and illustrated through run charts.
Results
To provide context for our results, as illustrated in Figure 2, it’s essential to highlight the trend in the percentage of seven-day outliers—these are patients who found themselves in a situation where they needed IV antibiotics and were at risk of prolonged hospitalization. Initially, the average percentage of these seven-day outliers stood at 22.8%. However, during the project’s kickoff phase, spanning from November 2020 to October 2021, a significant and noteworthy decrease was observed, bringing this percentage down to 12.4%. This substantial reduction demonstrated the early positive impact of the intervention.
Building on this success, the positive trend continued after a full year of the project’s implementation, from November 2021 to September 2022. During this period, the average percentage of seven-day outliers further decreased to just 8%. This sustained improvement highlights the effectiveness of the interventions and their ability to create lasting change, ultimately benefiting patient care and reducing the burden of prolonged hospitalization.
These results underscore the significance of the OPAT project in addressing the challenge of extended hospital stays for patients requiring IV antibiotics. The data reflects a substantial and positive shift in patient outcomes, reinforcing the project’s value in terms of both quality and efficiency in healthcare delivery.
The figures above reflect the number of saved days through OPAT (Figure 3). The decrease in inpatient days has a great impact in operational gains, amounting to a total of 2,019,000 riyals ($540,000) (Figure 3.1).
To demonstrate clinical viability, the OPAT Compliance in Figure 4 presents project sustainability. Only one patient did not show during the OPAT course. Further, there were no readmitted cases due to OPAT complications (Figure 5).
Discussion
Summary
The OPAT project at AHAFH has realized its objectives across three pivotal dimensions: clinical, operational, and financial success. This achievement is marked by the establishment of a secure and patient-friendly alternative for managing patients, and it is deemed highly successful due to remarkably low dropout and complication rates, virtually amounting to nil.
The success of this project serves as a promising model for healthcare providers throughout Saudi Arabia. The favorable results and insights derived from this initiative are anticipated to inspire and empower other healthcare service providers, clinicians, healthcare managers, and policymakers to replicate and adapt similar programs within the broader Ministry of Defense Health Services (MODHS) framework.
This successful implementation of the OPAT project not only improves the quality of care for patients, but also demonstrates the potential for enhancing healthcare delivery, efficiency, and cost-effectiveness. It is a testament to the capacity of healthcare institutions to innovate and adapt, ultimately benefiting the well-being of patients and the broader healthcare system.
Interpretation
The association between OPAT interventions and outcomes is causative in nature, with these interventions directly influencing various aspects of healthcare. OPAT interventions lead to a significant reduction in hospital LOS by allowing patients to receive IV antibiotics in outpatient settings, directly lowering healthcare costs, and improving the patient experience. Additionally, they reduce the risk of healthcare-associated infections and enhance resource efficiency by freeing up hospital beds. These interventions drive positive outcomes by reducing the need for inpatient care and improving the overall quality of care for patients requiring intravenous antibiotics.
The comparison of OPAT results with findings from other publications reveals consistent trends and outcomes. Many studies in the existing literature support the positive impact of OPAT interventions on reducing hospital LOS and healthcare costs. These results align with the broader body of evidence that demonstrates the effectiveness of OPAT in enhancing patient care, optimizing resource allocation, and minimizing the risks of hospital-acquired infections. The synergy of findings from various publications strengthens the case for OPAT as a valuable approach in healthcare, emphasizing its potential to reduce the burden on inpatient facilities while improving patient outcomes.
The impact of the OPAT project on both people and healthcare systems has been substantial. From a patient perspective, the project has translated to more convenient and comfortable treatment options, reducing the need for extended hospital stays. This has improved the overall quality of care and patient satisfaction. Additionally, the shortened LOS has allowed patients to return to their daily lives more quickly, minimizing disruptions and improving their well-being.
From a healthcare system perspective, the OPAT project has led to a more efficient allocation of resources, with a significant reduction in the utilization of inpatient beds. This has not only reduced costs, but also eased the strain on hospital facilities, making them available for more critical cases. Moreover, the project has been instrumental in decreasing the risk of hospital-acquired infections, enhancing patient safety, and streamlining the administration of antibiotics. Overall, the OPAT project has demonstrated a positive impact on people’s lives by offering improved care and on healthcare systems by optimizing resource utilization and reducing the burden on inpatient facilities.
Divergences between the observed outcomes and the initially expected results in the context of the OPAT project can be attributed to various factors, including the influence of the healthcare environment. These variations primarily stem from the inherent variability among patients, with each individual’s response to OPAT being influenced by their specific health conditions, treatment adherence, and personal characteristics. The clinical complexity of patients, notably those with intricate conditions, can also contribute to differences in outcomes, as they might necessitate extended antibiotic therapy or present challenges in transitioning to outpatient care. Furthermore, the level of patient adherence to OPAT treatment plans plays a crucial role, with variations affecting treatment effectiveness and LOS. Discrepancies in healthcare infrastructure, resources, and established OPAT programs can impact project outcomes. Additionally, regional variations in healthcare practices, patient expectations, and cultural factors within different healthcare contexts can lead to differing results. Data collection and analysis methods, as well as unforeseen challenges, such as changes in infectious agents or antibiotic resistance patterns, can further contribute to these divergences. Acknowledging and addressing these factors is crucial for refining OPAT interventions and enhancing patient care.
Limitations
The limitations of OPAT are linked to certain challenges that affect its practicality and efficacy. One significant constraint is the need for patients to return to the hospital for medication administration, which can be particularly problematic for individuals with limited access to transportation or those residing far from the healthcare facility. While there is an ambulance service available for patients without other means of transportation, its effectiveness depends on the availability of ambulances and healthcare personnel. This highlights the need for efficient logistics and coordination to ensure that patients can access OPAT services, especially in cases where transportation is a barrier to care. Additionally, a notable limitation is the focus on patients who require medications administered twice a day, which means that those who need antibiotics more frequently may not benefit from OPAT. This restriction can lead to the exclusion of patients whose treatment could potentially be managed through outpatient care. These limitations underscore the need for a patient-centered approach to ensure that OPAT is accessible and suitable for a wide range of individuals with varying needs and conditions.
Conclusions
In conclusion, the OPAT project has shown promising results in improving the quality of care and the efficiency of healthcare delivery. By enabling patients to receive intravenous antibiotics in an outpatient setting, the project has reduced the burden on hospital beds and improved patient safety and satisfaction. While there are some limitations and challenges, such as transportation issues, the OPAT project offers a valuable alternative to inpatient treatment for suitable patients. With further refinement and expanded criteria, OPAT has the potential to make a significant positive impact on healthcare systems and patient outcomes. It represents a noteworthy step towards providing effective and patient-centered care, aligning with the broader goals of enhancing healthcare quality and resource efficiency.
Acknowledgements
The authors would like to acknowledge the medical, nursing, and pharmacy staff of Al Hada Armed Forces Hospital for their involvement in this project, with special mention to members of the Infectious Disease team, physician and nursing champions, multidisciplinary team, and emergency department. We also would like to acknowledge the medical director and hospital director for their sponsorship and executive leadership to implement this project.
Disclosure
The authors declare that they have no relevant or material financial interests.
About the Authors
Jean Barrientos De Asis (jeandeasis07jed@gmail.com) is a registered nurse with licenses in the Philippines, Saudi Arabia, and New York, USA. She possesses a bachelor’s degree in biology and nursing, along with a Master of Arts in nursing. Furthermore, she is a certified professional in healthcare quality and holds the esteemed designation of a Lean Six Sigma Master Black Belt. In her current role as a nurse specialized in emergency nursing, she actively contributes to ensuring the alignment of patient safety and actively participates in quality improvement projects at the Armed Forces Hospitals Taif Region.
Abdulrahman Al Ghamdi serves as a consultant in pediatric infectious diseases at the Armed Forces Hospitals Taif Region (AFHTR). He holds a leadership role in the outpatient parenteral antimicrobials therapy (OPAT) project program at AFHTR and is the chief of the local committee for the Saudi Pediatric Residency Program in the Western region. Additionally, he is the head of the Clinical Dietitian Department.
Muhammad Hasan Abid holds the role of regional head for Patient Experience and Continuous Quality Improvement at the Armed Forces Hospitals Taif Region (AFHTR). As a patient safety specialist, he is additionally recognized as an Institute for Healthcare Improvement Fellow and Mentor. He assumes a leadership position, ensuring the alignment of quality improvement and patient safety projects with the strategic goals for enhancing patient experience at AFHTR.
Jamal Al Nofeye currently holds the position of regional director for Continuous Quality Improvement and Patient Safety in the Taif Region, Saudi Arabia. He serves as a board member for the Taif Health Cluster. As a physician, he has earned dual master’s degrees, including an Executive Master of Business Administration (Honors) and a Master of Science in healthcare quality and safety from Harvard Medical School. Additionally, he is a certified project manager.
Reynan Subahani Bautista is a licensed nurse and a dedicated member of the Continuous Quality Improvement and Patient Safety workforce. He obtained his Bachelor of Science in nursing in 2007 from Western Mindanao State University. Presently, he is actively working towards a master’s degree in nursing, specializing in nursing administration, at the Philippine Women’s University.


.jpeg)

.jpeg)
.jpeg)

.jpeg)

.jpeg)
.jpeg)