Introduction
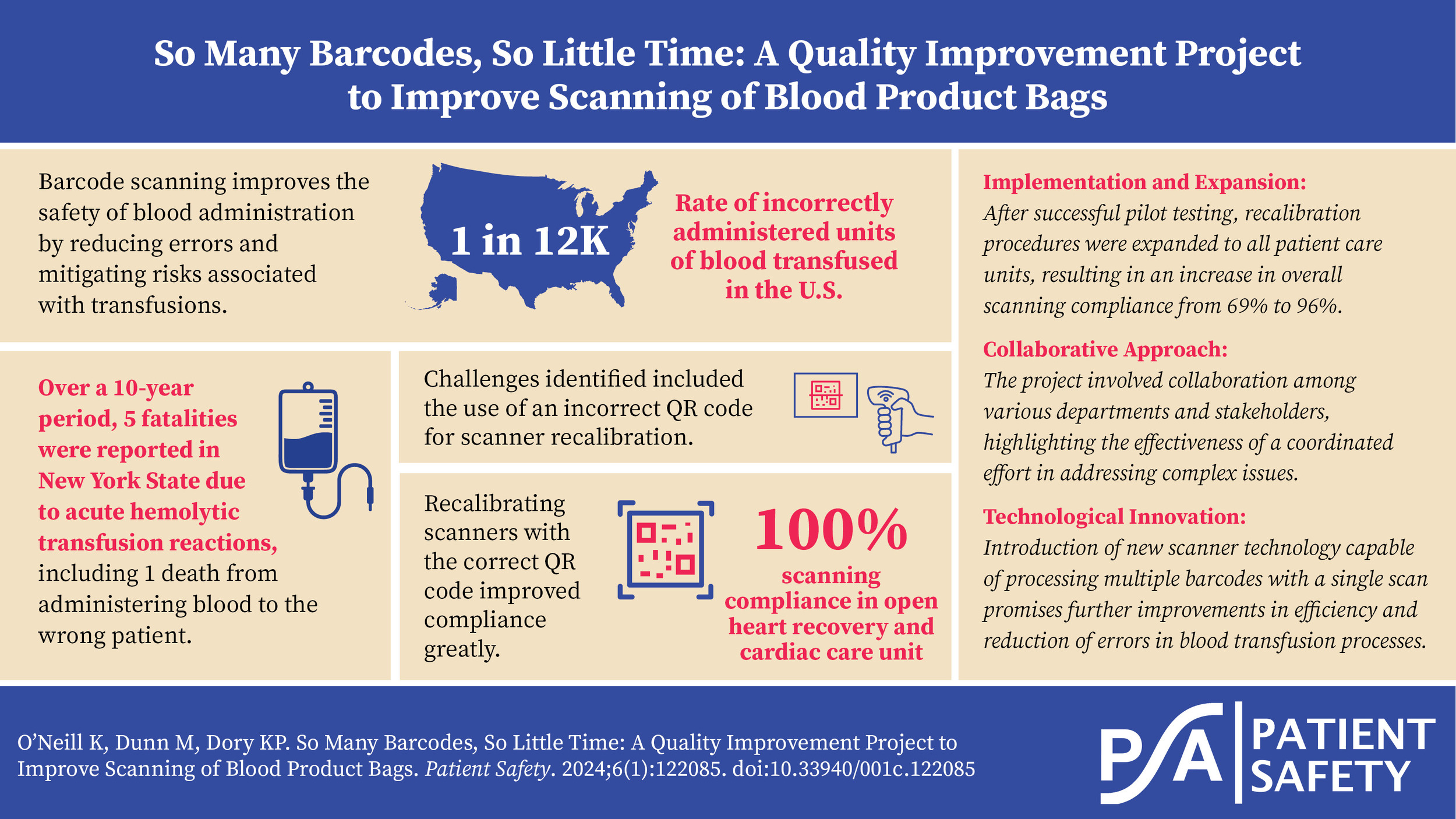
Blood administration is the transfer of blood or blood components from one person (the donor) into the bloodstream of another person (the recipient). This may be done as a lifesaving maneuver to replace blood cells or blood products lost because of bleeding, to improve clotting time, and to improve the ability of the blood to deliver oxygen to the body’s tissues. Incorrect administration of blood is estimated to occur once in every 12,000 units transfused in the United States.1 In an analysis conducted by the New York State Department of Health2 over a 10-year period, there were five fatalities, representing 4% of patients experiencing acute hemolytic transfusion reactions. This includes one death due to administering blood to the wrong patient, translating to an average of 0.5 incidents per year, or one death per 1.8 million transfusions. The implementation of blood bag scanning protocols serves as a robust safety measure in the hospital setting. However, if blood products do not scan, the registered nurse (RN) must manually override the process, which is not best practice. In addition, this stringent verification process culminates in the timely documentation of the procedure in the medical record.
The blood administration process is not foolproof; however, the frequency of avoidable transfusion fatalities attributable to misidentification of the blood product can be averted by using barcode technology.3 Scanning of blood products using barcode scanning technology improves the safety of blood administration and mitigates the risk of adverse reactions and transfusion-related complications.4
The Joint Commission (TJC) defines any blood or blood product transfusion error which results in death, permanent harm, or severe harm as a sentinel event.5 Failure to properly identify patients prior to administering blood or blood products can be a deleterious factor in the clinical setting. TJC recommendations to reduce risk include training of staff in appropriate transfusion-related procedures, revising the staffing model, enhancing the patient identification procedure, enhancing computer support, and redesigning the environment.
The Association for the Advancement of Blood & Biotherapies (AABB) mandates certain requirements for labeling and barcode technology of blood products, as they play a crucial role in transfusion medicine and enhancing the identification, storage, tracking, and distribution of blood and blood products.6 This technology improves efficiency, traceability, accuracy, and safety while reducing operational costs.
Essential label components include a unique facility identifier, donor-related lot numbers, product codes, and ABO and Rh donor information. Blood transfusion bags will therefore have four to six barcode labels on the front of the bag (see Figure 1). A barcode reader/scanner may have difficulty focusing on one particular barcode or read the barcode that is easiest to scan; consequently, nurses find themselves making multiple attempts to successfully scan a blood bag, which potentially leads to delays in patient care.
This quality improvement (QI) study describes our efforts to enhance the workflow efficiency of the blood administration process by the RN. We utilized a multipronged approach to identify and implement solutions to improve the accuracy of blood product scanning by the nurse.
Background
In late 2020, a persistent challenge emerged within our hospital. Nursing staff encountered difficulties when scanning blood products, prompting an ongoing cycle of deflecting blame between the Blood Bank, Nursing, and Informatics departments. It became evident that we needed a collective effort to address the root causes and pave the way for lasting solutions.
The identified issues were multifaceted. Scanning blood products presented unique challenges, given the multiple barcodes on each product and the complexity of the blood product administration workflow in the electronic health record (EHR). To ensure accuracy, nurses were required to scan three distinct labels: lot number, expiration date, and unit number. Initially, it was believed that these hurdles were primarily related to user proficiency, leading to the creation of practice alerts aimed at increasing awareness of the issues for our nursing staff.
Aim
The aim of this QI project was to achieve a 100% barcode scanning adherence of blood bags scanned at the bedside.
Methods
In our pursuit of bringing about change and improvement, we adopted the Plan-Do-Check-Act (PDCA) methodology. This comprehensive approach allowed us to methodically plan, execute, assess, and refine our efforts, leading to successful outcomes.
As this project was QI-related and no patient identifiers were included in the analysis, this study was deemed exempt by the Mount Sinai Health System Institutional Review Board.
Planning Phase (Plan)
Our journey commenced in late 2020 when we initiated interprofessional meetings that brought together representatives from the Blood Bank, Nursing, Quality Improvement, and Informatics departments. The aim was to foster collaboration and synergize our collective efforts. During this period and extending into early 2021, we took several critical steps:
-
We created a Practice Alert (a brief educational communication disseminated to nurses via email and print format) to increase awareness among nursing staff regarding proper scanning techniques, emphasizing its importance to our patients’ safety (see Figure 2).
-
An integral aspect of our planning phase involved the meticulous review of barcode scanning results for 2020. This data was aggregated by unit and department, with particular attention to compliance rates. Notably, the Department of Anesthesia stood out with a remarkable 100% compliance rate.
-
In early 2021, we decided to delve deeper into the intricacies of our practices. This involved shadowing anesthesiologists to gain insights into their workflows. To our surprise, their workflow closely resembled that of our RNs.
Execution Phase (Do)
We then embarked on the execution phase. During this period, we actively consulted with our scanner equipment vendor, Derive Technologies, and the manufacturer, Zebra Technologies, to identify potential root causes contributing to our challenges. An important discovery emerged during this process—we had been using an incorrect QR code for scanner recalibration (see Figure 3). With this knowledge, we took swift action:
-
We recalibrated scanners in the open heart recovery (OHR) and cardiac care unit (CCU) using an updated QR code.
-
The OHR/CCU is a 26-bed, adult critical care unit focusing on patients with critical coronary care issues, immediate postoperative open heart surgery patients, and acute stroke patients.
-
The OHR/CCU administers the most units of blood/blood products, second only to the Department of Anesthesia.
Assessment Phase (Check)
By mid-2021, we had transitioned into the assessment phase. Here, we closely monitored the effects of our intervention on the OHR/CCU. We were keen to observe any improvements in barcode scanning compliance. After just one week of pilot testing, our efforts yielded positive results, with noticeable enhancements in compliance rates (see Figure 4 and Figure 5).
Refinement Phase (Act)
Armed with our findings and with a renewed commitment to our mission, we entered the refinement phase. Our actions were twofold:
-
We initiated a comprehensive recalibration process for scanners on all units to ensure uniformity and sustained accuracy.
-
Additionally, calibration cards were replaced on all workstations on wheels (WOWs), optimizing our scanning systems across the board.
This methodical approach, guided by the PDCA methodology, empowered us to drive effective change and significantly improve our barcode scanning processes when administering blood products.
Setting
This QI project was conducted at Mount Sinai Morningside, one of eight hospital campuses that comprise Mount Sinai Health System in New York, along with a school of medicine and a school of nursing. Mount Sinai Morningside is a 495-bed, acute care hospital located within the Morningside Heights neighborhood in New York City and offers multiple specialties, including a Level II trauma center, bariatrics, cardiology, cardiac surgery, and internal medicine.
Our EHR system is supported by Epic EHR, which is a cloud-based EHR system and one of the major hospital EHRs in the United States. Epic was fully implemented at Mount Sinai Morningside in 2018. To enhance patient safety and reduce the chance of errors, barcoding technology was implemented for specimen collection, medication administration, breast milk administration, point-of-care testing, and blood and blood product administration. Our Epic EHR supports this technology in order to overcome manual processes and provide real-time feedback and data analysis.
Results
Consequently, based on prior experience, the Informatics team harbored a persistent sense that the problem was more fundamental than user-related issues. It was at this critical juncture that we decided to enlist the expertise of the scanner equipment vendor, Derive Technologies, and the manufacturer, Zebra Technologies. This partnership would prove pivotal in unraveling the intricacies of the scanning issue.
Upon consulting the manufacturer, we were presented with a recommendation that, while technically viable, seemed impractical. It involved reprogramming each scanner individually, a time-consuming endeavor with limited appeal. Our search for a more efficient solution led us to a remarkable discovery: the manufacturer offered two QR codes for scanner recalibration. This prompted a vital question: “What if we had been using the wrong QR code all along?” To test this hypothesis, we embarked on recalibration with the alternative QR code.
The OHR/CCU was selected for this crucial test phase, not only due to its high blood product usage, but also because the scanning issue had a significant impact on its daily operations. Scanning compliance on the OHR/CCU ranged from 70% to 93%, indicating the extent of the problem (see Figure 4). The enthusiasm and collaboration of the staff and nurse manager on the unit were instrumental in the success of this endeavor.
After we recalibrated the scanners with the new QR code in April 2021, the outcomes were nothing short of remarkable. In May 2021, the OHR/CCU reached the pinnacle of 100% compliance, a staggering 43% increase compared to the results observed in January 2021 (see Figure 6). With this milestone, we knew we had the solution in our hands, and the urgency to expand it to other units became apparent.
The solution expansion began in May 2021 when new recalibration cards were ordered and distributed to the more than 20 remaining patient care/procedural units, including the emergency department and post-anesthesia care unit (PACU). Prior to the arrival of the cards, a proactive approach was taken. Nurse managers were provided with the QR code and recalibrated the WOWs on their units, ensuring minimal downtime. The new calibration cards not only were a distinctive color, but also featured a date, streamlining the recalibration process.
Engaging stakeholders and staff was a testament to the power of bringing subject matter experts together, focusing on a solution rather than workarounds, and ensuring that the solution was disseminated comprehensively. This collective effort contributed to the remarkable improvement in overall scanning compliance, which increased from 69% in January 2021 to an impressive 96% in May 2021.
Conclusions
Patient safety may be compromised when there is improper barcode scanning when administering blood products. This quality improvement initiative demonstrated the importance of collaborating with the right stakeholders in problem-solving clinically relevant processes. Use of the PDCA cycle to improve the barcode scanning of blood products and identifying end-user needs was critical to the success of this project. Increase in efficiency of the nursing workflow (see Figure 7) and replicability of the solution are essential to optimizing safe blood administration practices.
While the majority of our efforts resulted in substantial progress, a temporary decrease in compliance emerged in February 2022. Despite thorough investigations, no concrete reason could be attributed, leading us to ascribe it to an isolated instance of user error. The unwavering commitment to solving this issue remains steadfast, a testament to the resilience and adaptability of our healthcare system. The increase in compliance with barcode scanning of blood bags following the recalibration of the scanners was a significant achievement at Mount Sinai Morningside and was replicated at another facility within our healthcare system. As there are patient safety and financial implications for improper barcode scanning when administering blood products, we continue to review barcode scanning results on a periodic basis to evaluate for sustained improvement.
In 2021, Zebra Technologies announced that it had introduced a customized handheld scanner to expedite the processing of multiple barcodes on blood bags. This technology allows the scanner to recognize and capture the multiple barcodes on a blood bag with a single scan. The hospital where this scanner was introduced reported a fifty percent increase in efficiency of blood transfusions while mitigating human errors.7 In conclusion, as technology continues to evolve, ongoing innovation and the need to safeguard patient safety holds the promise of further enhancing blood transfusion.
Disclosure
The authors declare that they have no relevant or material financial interests.
About the Authors
Kelly O’Neill is an associate director of Nursing Informatics at Mount Sinai Health System with a robust background in medical-surgical nursing and over seven years of experience in nursing informatics. Dedicated to patient safety and workflow efficiency, O’Neill bridges clinical needs with information technology solutions to optimize electronic documentation and enhance care delivery. She holds a Master of Science in nursing (executive leadership) from Felician University and is committed to advancing nursing innovation and informatics to drive transformative change in healthcare.
Michelle Dunn (michelle.dunn@mountsinai.org) is an accomplished healthcare professional with extensive experience in patient-centered care and nursing quality improvement within adult acute care settings. With a career spanning over four decades, Dunn has developed and led numerous initiatives to enhance patient safety, quality, and performance. Currently serving as the director of Nursing Quality Improvement at Mount Sinai Morningside and Mount Sinai West, Dunn excels in driving hospitalwide performance improvement and ensuring compliance with regulatory standards. Her expertise in nursing quality metrics, Lean Six Sigma Green Belt certification, and proficiency in data analysis and reporting have significantly contributed to improved patient outcomes and operational efficiency. She has a master’s degree in nursing from the University of Phoenix and a bachelor’s from Long Island University.
Kathleen Parisien Dory is a director of Nursing Education, Professional Practice and Research at Mount Sinai Health System. She is a nurse leader with 25 years of experience in medical-surgical nursing, education, and professional practice. She is committed to high-quality patient care, implementation of evidence-based practice, and service excellence. She is recognized for being a strategic systems thinker, developing high-performing teams, executing large scale hospitalwide training and evidence-based solutions, and leading change at the system level. She holds a Bachelor of Arts from Mount Holyoke College and a Bachelor of Science and Master of Arts in nursing from New York University.




_prior_to_implementation_of_the_solution.jpeg)
_after_implementation_of_the_solution.jpeg)
_blood_scanning_compliance_ohr_ccu_and_mount_sina.jpeg)




_prior_to_implementation_of_the_solution.jpeg)
_after_implementation_of_the_solution.jpeg)
_blood_scanning_compliance_ohr_ccu_and_mount_sina.jpeg)
