Introduction
Problem description
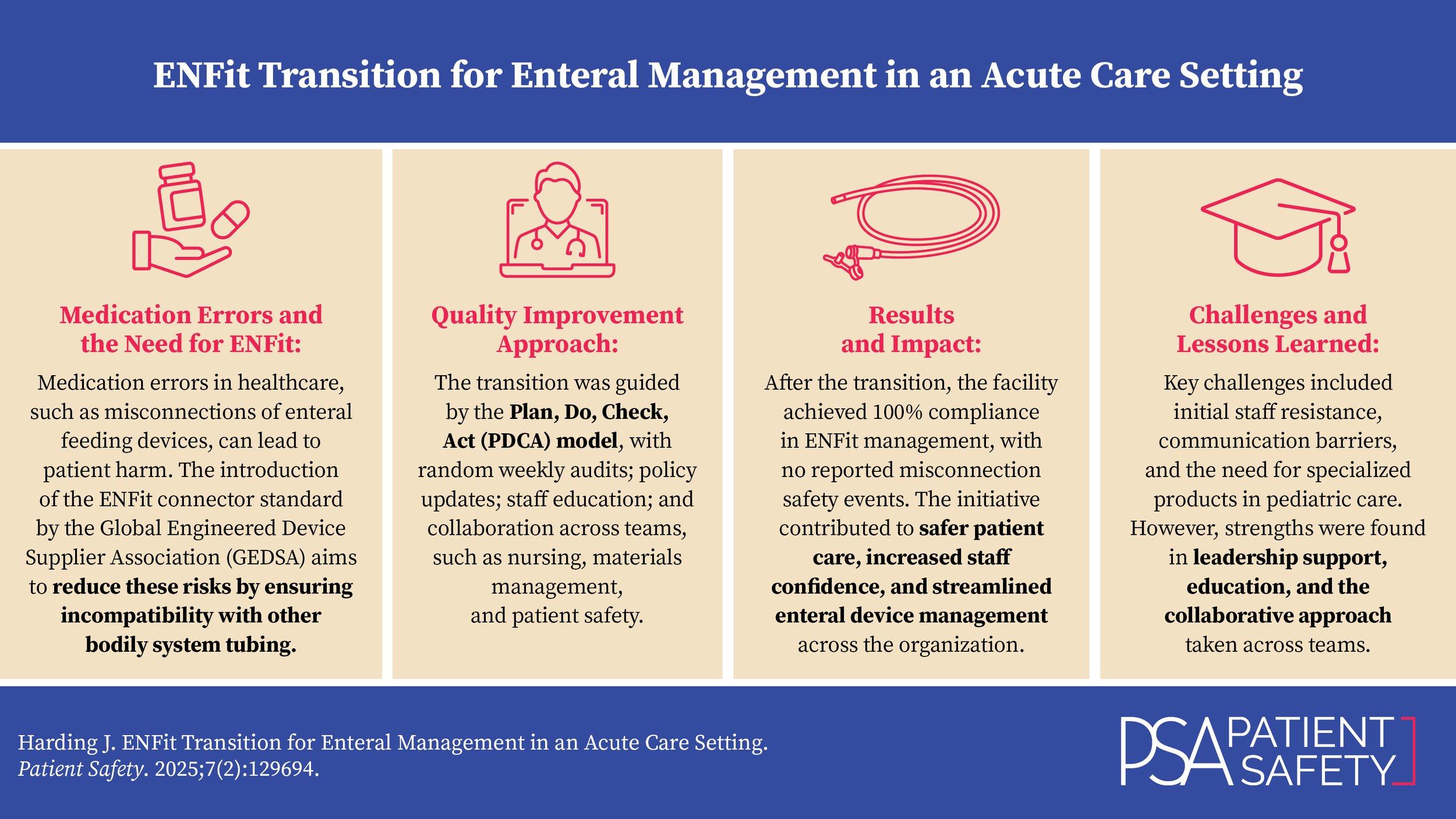
Medication errors within healthcare occur in many forms, such as a medication given to the wrong patient, the patient receives the incorrect medication, the patient receives the incorrect dose (incorrect strength or quantity) of medication intended, or the patient receives a medication by the incorrect route. While medications inadvertently administered by an incorrect route is only a subset of the types of medication errors that occur throughout healthcare, results of wrong-route medication errors can lead to patient harm with limited options for corrective actions.1
Global Engineered Device Supplier Association (GEDSA), a federal, tax-exempt, nonprofit trade association, introduced an advancing patient safety initiative to globally coordinate the implementation of small bore feeding tube connectors in 2015. These feeding tube connectors are developed through the ISO 80369 series standards to be mechanically incompatible with other bodily system tubing connections (like intraveneous connections).2 The bodily system–specific connectors would therefore reduce the risks of misconnections with other bodily system devices and further reduce patient harm or death.2 The bodily system connections specific to enteral devices through the GEDSA standard design are called ENFit.
Until the ENFit enteral system was designed, the United States utilized traditional legacy enteral feeding systems designed with a traditional luer connector with a male-to-female orientation. Legacy connectors are compatible with other therapy devices, such as intravenous (IV) ports, catheters, and nonenteral tubing.3 The ENFit features a nontraditional female-to-male orientation on enteral feeding devices (Figure 1).3 Additionally, manufacturers of enteral products stopped manufacturing legacy feeding tubes as of July 2021, and further stopped manufacturing feeding tube sets with the transition connector as of January 2022. The transition connector was a provisional strategy to help complete the conversion of enteral feeding tube devices to the ENFit orientation.
Setting
This quality improvement project was completed in a Level I trauma center in south-central Pennsylvania, a 525-bed facility that serves inpatient and observation acute patient admissions, as well as outpatient services of dialysis, general and orthopedic surgery, endoscopy, interventional radiology, radiology, and heart and vascular services. This project began in March 2022 and was later rolled out to all care areas where patients may present with enteral feeding devices, including ambulatory sites.
Available knowledge
Beginning in January 2022, manufacturers stopped manufacturing enteral feeding sets with a transition connector. The transition connector allows the enteral feeding set to be directly connected to a non-ENFit enteral device. To assess the current state of ENFit versus non-ENFit feeding devices being managed, three months of random weekly visual audits of patients with feeding devices admitted to the acute care setting were conducted.
After completion of random visual audits, a recommendation was made to transition to the insertion practice of only inserting ENFit-compatible feeding devices, with the additional practice of moving to ENFit management of all feeding devices while a patient is admitted in the acute care setting. The current state had shown that an average of 40% of enteral devices were considered ENFit compatible in the presentation of management (Figure 2). Many facilities are in the developmental and growing process to become a high reliability organization (HRO), which focuses on patient safety in real-time with emphasis on understanding general operations, desired steps of processes, and resilience from adverse events that do occur.
The facility’s continued journey to high reliability concluded that there was a need to transition enteral management to only ENFit-compatible devices to promote patient safety and reduce harm to patients related to misconnections to other bodily system devices. This distinct statement was a recognition that the facility would undergo an organizational transition that pertains to nursing practice and patient care environments, as well as recognizing institutional policies to be changed, procedures to be adjusted, and practices to be identified for change.
When GEDSA introduced the ENFit design in 2015, the facility started to introduce ENFit-related products into the acute care setting, including cataloging ENFit enteral feeding devices, as well as ensuring the presence of the transition connector and the ENFit Lopez Valve (a three-way stop valve with ENFit connections). Through the beginning of 2022, the facility had also held on to legacy (non-ENFit) feeding devices, while continuing insertion practices of mainly legacy feeding devices.
Rationale
Gastrointestinal (GI) feeding tubes within the inpatient acute care setting can present as traditional legacy tubing or may now present with ENFit connections, due to a worldwide manufacturer transition to ENFit connections for enteral devices to promote patient safety and reduce misconnections. Both styles of GI feeding tubes (traditional legacy and ENFit) are managed differently, with different syringe sets and potential adapters, allowing for significant variation in management for inpatient nurses. Manufacturers have developed transitional adapters to allow for ENFit management of any enteral feeding tube device, to reduce variability in management, and to start all enteral device management as ENFit.
Aim
To achieve a full organizationwide product transition to all ENFit product use for enteral device management, and to obtain 100% ENFit management of enteral feeding devices for feeding or medication administration by December 31, 2022, and prevent enteral device–related patient safety events.
Objectives
Understand the consideration for an ENFit conversion to promote patient safety around enteral devices and reduce misconnections.
Understand the organization’s impact on ENFit conversion related to product transitions and supportive education.
Understand troubleshooting concerns after ENFit conversion to ensure continued patient safety.
Methods
Context
The purpose of an ENFit conversion is to reduce the variety in management styles for enteral feeding devices and to complete product transitions for enteral device management, to coincide with manufacturer development and transition to ENFit enteral products. To address this, a multidisciplinary team utilized the Plan, Do, Check, Act (PDCA) model to guide a transition to ENFit enteral device management.
Interventions
The initial process used to determine the depth of the project included a random audit of approximately 5–10 enteral devices within the inpatient setting every week for three months to determine the current state of management variability. Additionally, before the project began there was a procedural change to only insert ENFit enteral feeding devices within procedural areas. After two weeks of audits the quality specialist and clinical nurse specialist fellow recommended a transition to all ENFit management, as the variety of enteral tube management and presentation was significant. Additional requests for approval from governing bodies, such as Value Analysis, Patient Safety, and Risk, were required prior to making a full transition to ENFit-compatible management for all enteral devices.
After three months of weekly audits to visualize enteral devices, the project focused on enteral device adapters and assessing any additional needs for products to ensure 100% ENFit enteral device management. The largest product change included a Salem Sump decompression tube change to an ENFit-compatible device (Salem Sump with ENFit multifunctional port) as well as an ENFit-compatible drainage bag for decompression for a feeding tube.
Other processes working towards the transitional phase included working with vendors to assess adapter needs, collaborating with Materials Management to work with the vendor on additional products needed, coordinating par levels in all areas affected, reviewing the GI tube nursing policy for updates, educating clinical nurse specialists and clinical educators of the Nursing Professional Development (NPD) team to act as super users of the new Salem Sump product, developing a GI Tube management guide for Nursing reference, communicating the product change update before the go-live date, ensuring every inpatient nursing unit had a sample of the new Salem Sump product to visualize and feel before the go-live date, and coordinating with storeroom management on the go-live date and expected completion date. After the go-live date, audits were completed to assess product changes and implementation.
Required changes
Based on the analysis of the depth of the quality improvement project, several changes were required for implementation throughout the facility by the interdisciplinary team members (Table 1).
Study of the Interventions
Outcome measures
The data collection for process improvements was done using Microsoft Excel to track the percentage of compliance per week of visual audits. The GI/General Surgery quality specialist also conducted audits at random when NPD staff and other healthcare leaders asked clarifying questions.
Process measures
Each of the changes required was assessed by qualitative or quantitative measures. The compliance with the use of each of the changes was measured by either continual audits until 100% compliance was obtained, or by continued discussion with corresponding teams and personnel until the change was conceptually achieved. Equally important were the subjective impressions of the frontline staff on the feasibility and success of each change that was required.
Analysis
The outcomes of the project were analyzed by review of audit compliance and with random audit check-ins with specific changes.
Results
Prior to the ENFit transition, on average 40% of enteral devices were considered ENFit-compatible for management purposes (Figure 2). After the full organization ENFit product transition, the collaborative approach resulted in 100% compliance in ENFit enteral device management (Figure 3).
Additional random audits conducted still resulted in safe ENFit management of devices and only required reiteration of resources available for reference for proper ENFit management. There have been no reported misconnection safety reports made related to enteral devices since the ENFit enteral device transition occurred.
Discussion
Summary
During this quality improvement initiative, anticipated results were achieved to obtain 100% ENFit management of enteral feeding devices for feeding or medication administration by December 31, 2022. The implementation of all ENFit-related feeding devices and associated adapters or products has gained nursing interest due to the importance of preventing misconnections with other bodily system devices and has reduced the variability of enteral device management to ENFit only.
Interpretation
As seen in Figure 3, the improvement in compliance of ENFit management of enteral devices was progressive over time. By the nature of repeated audits and correcting any needed changes in real-time with appropriate personnel, it is very difficult to determine which changes were responsible for overall improvement and how much of each change contributed to the overall result.
The quality improvement team and interdisciplinary team members faced many challenges during the project. They included:
-
An initial lack of staff understanding of the importance of the change to ENFit for enteral device management.
-
A vast communication network within the organization, which made it difficult to ensure all staff that encounter enteral devices received the same information.
-
A lack of understanding of the full capacity that enteral products are utilized within the organization before the transition occurred.
An important issue that was addressed during the ENFit enteral product transition was the emphasis of reporting safety events. In the presence of patient safety events and in producing a culture of safety, best known as Just Culture, all healthcare workers should feel comfortable sharing details about near-miss or adverse event situations.4 Developing Just Culture requires relationship building with patients, staff, and the system, which is modeled on trust, open communication, and understanding that those closest to the work are the most knowledgeable and are essential to process improvement efforts.4 The facility continues with creating and strengthening an environment of Just Culture.
Strengths and lessons learned
The quality improvement team and interdisciplinary team members identified areas of throughput that were recognized as strengths through the ENFit transition, including:
-
Support and guidance from Patient Safety and Quality leaders.
-
Engagement with clinical educators and clinical nurse specialists.
-
Safety initiative practices for enteral devices were being implemented nationwide.
-
The entire approach involved a multitude of collaborations from various teams.
-
Nurses were educated or had their knowledge refreshed in a multimodal way, using competency days, one-on-one instruction during audits when needed, and online written communication/resources.
The quality improvement team and interdisciplinary team members also identified areas of throughput that were not initially accounted for in the original ENFit transition, including:
-
Adjusting code carts that supply Salem Sumps in the case of a patient needing intubation.
-
Pediatric considerations for smaller sizes of the Salem Sump with ENFit multifunctional port were not available below a 10 French size, requiring additional education and notification to the pediatric team on an ENFit replacement for the 8 Fr and 6 Fr Salem Sump.
-
The use of suction for decompression with percutaneous endoscopic gastrostomy tubes (PEGs), as well as nursing staff handling tubing to comply with physician orders to set PEGs to suction.
-
Bedside PEG procedures were being completed on nursing units, where the nursing unit had a separate supply of PEG kits that were not initially known to be included in par levels or areas of inventory.
-
Provider practice of inserting red rubber urinary catheters as a jejunostomy tube.
-
One enteral device manufactured not as ENFit, however, has an available ENFit adapter that can be placed after surgical placement, and the process to ensure that adapter is placed for every procedure.
Overall, viewing transitions as both a process and outcome means that the emphasis of the transition may equally shift between process and results, and back again, illustrated by fluid movement across time and through impact of the patient, staff, and system involved.5
Conclusions
One characteristic of transitions is that transitions are in essence positive.4 Continued and constructive communication are required to engage staff positively while providing ongoing support to instill confidence in all healthcare providers involved in the ENFit transition. Failure in communication has been seen as a large contributor to near misses and adverse events, specific to how, when, and by whom the communication is given.4
This initiative had a positive impact on patients, staff, and the organization as a whole. For patients, it reduced the ability of a device misconnection to occur with enteral devices, leading to safer, quality healthcare. For the staff, confidence in ensuring the safe management of patients with enteral devices can be transferred and applied to other areas of healthcare needs and improve job satisfaction. For the organization, reduced cost of product acquisition and use of proper enteral devices lead to improved patient satisfaction along with safe and quality healthcare.
Acknowledgements
The author would like to thank the director of Patient Safety and director of Quality for their support to initiate this quality improvement project. The author would like to thank the Nursing Professional Development team (nurse educators and clinical nurse specialists), Supply Chain Logistics team, GI & General Surgery Clinical Effectiveness Committee, Informatics team, and Nutrition team for their continuous collaboration throughout the quality improvement project transition. The author would especially like to thank the Pulmonary clinical nurse specialist fellow, the Emergency Department/Observation clinical nurse specialist fellow, the Perioperative Services clinical nurse specialist, the manager of Endoscopy, the administrative director of GI & General Surgery, the Materials Management analyst, the manager of Supply Chain Logistics and supervisor of General Stores, the medical director of Informatics, the supervisors of Clinical Nutrition, and the supervisor of Patient Education and Engagement for their kind assistance and collaboration to the quality initiative.
Notes
An international review board was not sought to review, as all the changes being implemented were widely accepted internationally. There was no control group, therefore no randomization, so no patients would be denied intervention when necessary.
All data relevant to the project are included in the article.
The Patient Safety Authority helped guide the initial draft of this manuscript.
Disclosure
The author declares that they have no relevant or material financial interests.
About the Author
Janelle Harding (janelle.paules@yahoo.com) is a registered nurse and clinical nurse specialist, with an associate nursing degree from Pennsylvania College of Health Sciences (now Saint Joseph’s University), Bachelor of Science in nursing from Millersville University, and a Master of Science in nursing as a clinical nurse specialist from West Chester University. Harding is currently enrolled in a doctorate of nursing practice program at West Chester University. Harding holds certifications in medical-surgical nursing, gerontology nursing, and adult-gerontological nursing from the American Association of Critical-Care Nurses (AACN) and a certification in professional healthcare quality from the Agency for Healthcare Research and Quality (AHRQ). Harding also teaches clinical hours part-time for Saint Joseph’s University within the associate nursing program. Harding’s work in quality focuses largely on healthcare system improvements to enhance healthcare quality, minimize risks, and optimize patient outcomes. Harding is committed to championing excellence in nursing practice and driving positive change within the healthcare system, one quality improvement initiative at a time.