Introduction
Problem Description
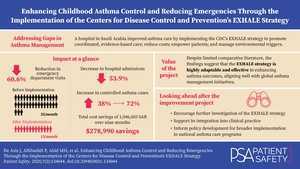
At Armed Forces Hospital, our team observed that 62% of asthmatic patients were uncontrolled in the year 2022. This represented 6% of the total monthly emergency department (ED) visits and 10% of the monthly pediatric hospital admissions. In addition, 60% of individuals referred to Pediatric Pulmonology were identified as asthma mimickers. This factor contributed to the extended third next available appointment (TNAA) for Pediatric Pulmonology, which was 23 days, surpassing the hospital’s targeted timeframe of 14 days, thus emphasizing the need for a thorough and qualitative approach in ensuring accurate diagnosis and proficient management.
Available Knowledge
Asthma is a significant global health issue characterized by chronic airway inflammation, resulting in recurrent episodes of wheezing, breathlessness, chest tightness, and coughing. This condition poses a considerable burden on individuals’ quality of life and healthcare systems due to frequent hospitalizations, ED visits, and medication costs. Asthma is ranked 16th among the leading causes of years lived with disability and 28th among the leading causes of burden of disease, as measured by disability-adjusted life years. Around 300 million people have asthma worldwide, and it is likely that by the end of 2025 a further 100 million may be affected.1 Also, asthma is associated with a significant number of deaths, with an estimated 455,000 asthma-related fatalities reported globally in 2019.2,3
In the Kingdom of Saudi Arabia (KSA), more than 2 million people struggle from asthma, and a considerable number of them experience uncontrolled symptoms that significantly diminish their quality of life.4,5 Annually, the cost of asthma was 88 million dirham in United Arab Emirates, 37.2 million U.S. dollars in the United States, and 27,014,735 Omani rials in Oman.6–8
The National Asthma Control Program (NACP) of the U.S. Centers for Disease Control and Prevention (CDC) developed a program called EXHALE, consisting of six strategies designed to enhance asthma control. These strategies are designed to complement each other to reinforce their impact. However, it’s worth noting that the full implementation of this program in the KSA has not been realized yet.
Rationale
Saudi Vision 2030 sets out the directions, objectives, and commitments that the KSA seeks to increase citizens’ well-being and quality of life. This can be achieved through promoting physical, psychological, and social well-being.
Asthma has a major impact on lifestyle and accounts for millions of missed school days each year. Thirty percent of young people with asthma have limited activity, compared with 5% of children without asthma.9
The implementation of the EXHALE strategy is driven by several compelling reasons in enhancing the control of asthma in patients, improving asthma management, and reducing the need for acute care services. This helps mitigate the economic burden associated with asthma-related healthcare utilization.
Aim
The key aim was to attain a 20% reduction in asthma-related visits to the ED, decreasing from 295 to 240 visits with a simultaneous reduction in hospitalizations due to asthma from 111 to 90 admissions by the end of September 2023.
Context
According to national guidelines, achieving comprehensive asthma control encompasses two primary facets. The first dimension involves reducing impairment, which entails preventing asthma symptoms, minimizing the utilization of emergency medications, maintaining optimal lung function, and ensuring individuals can participate in their regular physical activities while keeping up with their work or school attendance. The second dimension, on the other hand, focuses on reducing risk. This involves efforts to minimize the necessity for ED visits and hospitalizations by proactively preventing recurrent asthma attacks.
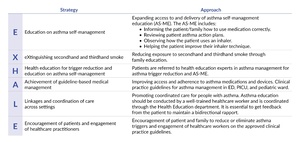
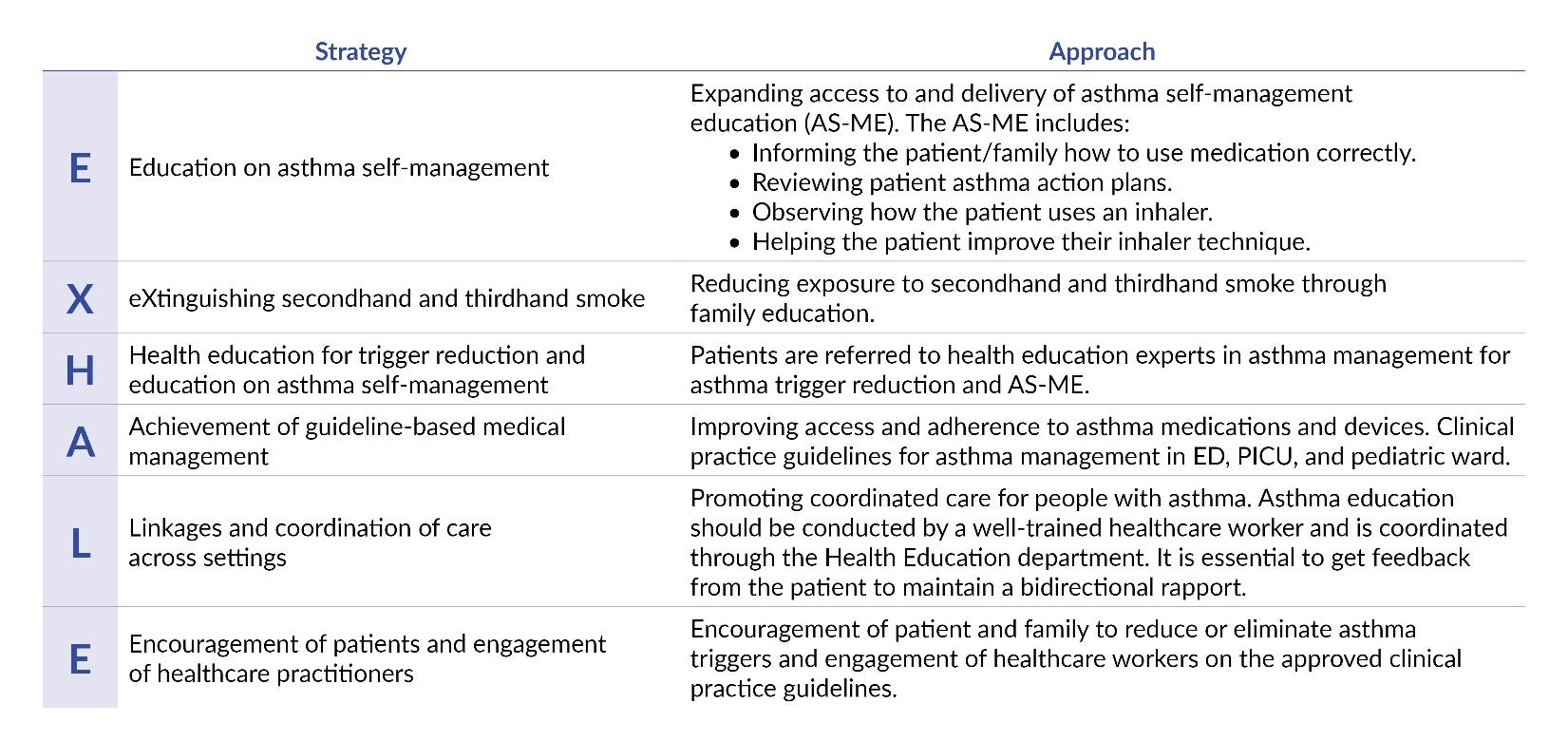
Our team adapted the CDC’s EXHALE strategy by replacing the final component—environmental policies to reduce asthma triggers—with a focus on encouraging patients and engaging healthcare practitioners. This adjustment ensured the strategy better aligned with local needs and cultural context.
Methods
Interventions
The project spanned from January to September 2023, during which baseline data were retrospectively gathered by reviewing the patient medical records admitted in the hospital due to asthma exacerbation.
The EXHALE project has been implemented holistically throughout the hospital, ensuring quality care from the moment a patient arrives at the ED, admission to the inpatient ward or pediatric intensive care unit (PICU), and follow-up in the Outpatient Department (OPD) clinic.
The team is composed of pediatric physicians, pediatric pulmonologists, health educators, patients, and caregivers and quality representatives.
The EXHALE strategy, reconfigured at our facility, encompasses a range of interventions that are fundamental for enhancing the quality of care provided to pediatric patients with asthma (Figure 1). This serves as the framework of the project containing the strategies and approach applied to pediatric asthma patients.
The asthma management process incorporates the EXHALE strategies at specific steps to ensure comprehensive care. First, all pediatric asthma patients with follow-up appointments or those admitted to the ED, inpatient units, or visiting the OPD are referred to Health Education for asthma self-management education (AS-ME) and guidance on reducing exposure to secondhand and thirdhand smoke. This includes proper medication use, reviewing action plans, improving inhaler techniques, and promoting smoke-free environments and smoking cessation.
Next, Health Education experts provide targeted support on asthma trigger reduction and reinforce self-management techniques, revisiting these if asthma remains uncontrolled. Evidence-based clinical practice guidelines (CPG) are implemented in the ED, PICU, and pediatric ward to standardize assessment, treatment, and monitoring. Coordinated care is promoted through the Health Education Department with patient feedback fostering bidirectional communication. Finally, patients and families are encouraged to minimize asthma triggers, while healthcare practitioners are engaged to adhere to approved CPG, ensuring consistent, evidence-based care and better outcomes.
The team has engaged in a structured process of Plan-Do-Check-Act (PDCA) cycles to optimize the implementation of the EXHALE strategy. Each cycle targeted specific aspects, from CPG implementation and asthma assessment forms to educational programs for patients, parents/caregivers, and collaboration with Health Education. These cycles demonstrated an adaptive approach, responding to initial successes, identifying challenges, and refining strategies for pediatric asthma management.
Study of the Intervention
Our measures focus on the key performance indicators (KPIs) on asthma-related hospitalizations, emergency department visits, and associated healthcare costs. These KPIs were reviewed and validated by the quality department of the hospital. Baseline data (January–December 2022) were collected and compared with the current data to effectively measure the strategy’s impact. The team meets on a monthly basis to discuss the results and identify the challenges and generate action plans.
Measure
In terms of outcome measures, we measured the percentage of ED visits attributed to asthma exacerbation, the admission rate due to asthma exacerbation, and the percentage of controlled asthma patients based on defined criteria. Patient experience was evaluated qualitatively through a consented survey.
For the process domain, we measured the compliance with CPG in the ED, PICU, and pediatric ward. Additionally, we collected data regarding compliance with OPD appointments, analyzed the percentage of unnecessary ED visits, and tracked the percentage of patients who received health education on asthma management. The waiting time for education among uncontrolled asthma patients and the percentage of patients demonstrating correct device use were also assessed as process indicators.
Balancing measures focused on ensuring accuracy in asthma diagnoses, examining the percentage of patients correctly diagnosed as having asthma in comparison to the total number of admissions due to asthma.
These measures collectively provide a comprehensive understanding of the strategy’s effectiveness in improving patient outcomes and optimizing processes in asthma management. The strategy enhances care by improving access through streamlined scheduling and referrals, ensuring adherence to clinical guidelines, and prioritizing AS-ME with trained educators. It also fosters coordination among multidisciplinary teams and implements regular monitoring to ensure seamless care transitions and effective tracking of patient progress. Additionally, families are educated on reducing asthma triggers to support better outcomes. By focusing on these processes, the strategy aims to reduce healthcare utilization, enhance patient and caregiver satisfaction, and drive continuous improvement through monthly evaluations.
Analysis
The project employed a quasi-experimental pre- and post-period design to assess the impact of the intervention. In this project, participants were not randomly assigned to groups, but rather, the study involved the introduction of an intervention and the comparison of outcomes before and after its implementation. The initial phase focused on gathering baseline data to understand the existing conditions related to the outcome variable. Subsequently, the intervention was introduced, and post-intervention data were collected to evaluate any changes in the outcome.
The quasi-experimental design allows for the assessment of the intervention’s effectiveness in a real-world setting. Random assignment might not be feasible or ethical, and thus, this design provides a practical way to measure the impact of the intervention. The comparison of pre- and post-period data helps in understanding whether the observed changes can be attributed to the intervention. However, it’s important to note that the absence of randomization introduces the possibility of nonequivalence between groups, and statistical methods are employed to control for potential confounding variables. While this design offers valuable insights into the intervention’s effects, making causal inferences requires careful consideration of alternative explanations for any observed changes.
Ethical Considerations
As per hospital policy, Institutional Review Board (IRB) approval was not required because this was a quality improvement initiative.
Results
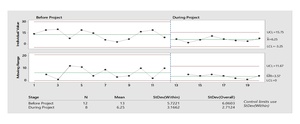
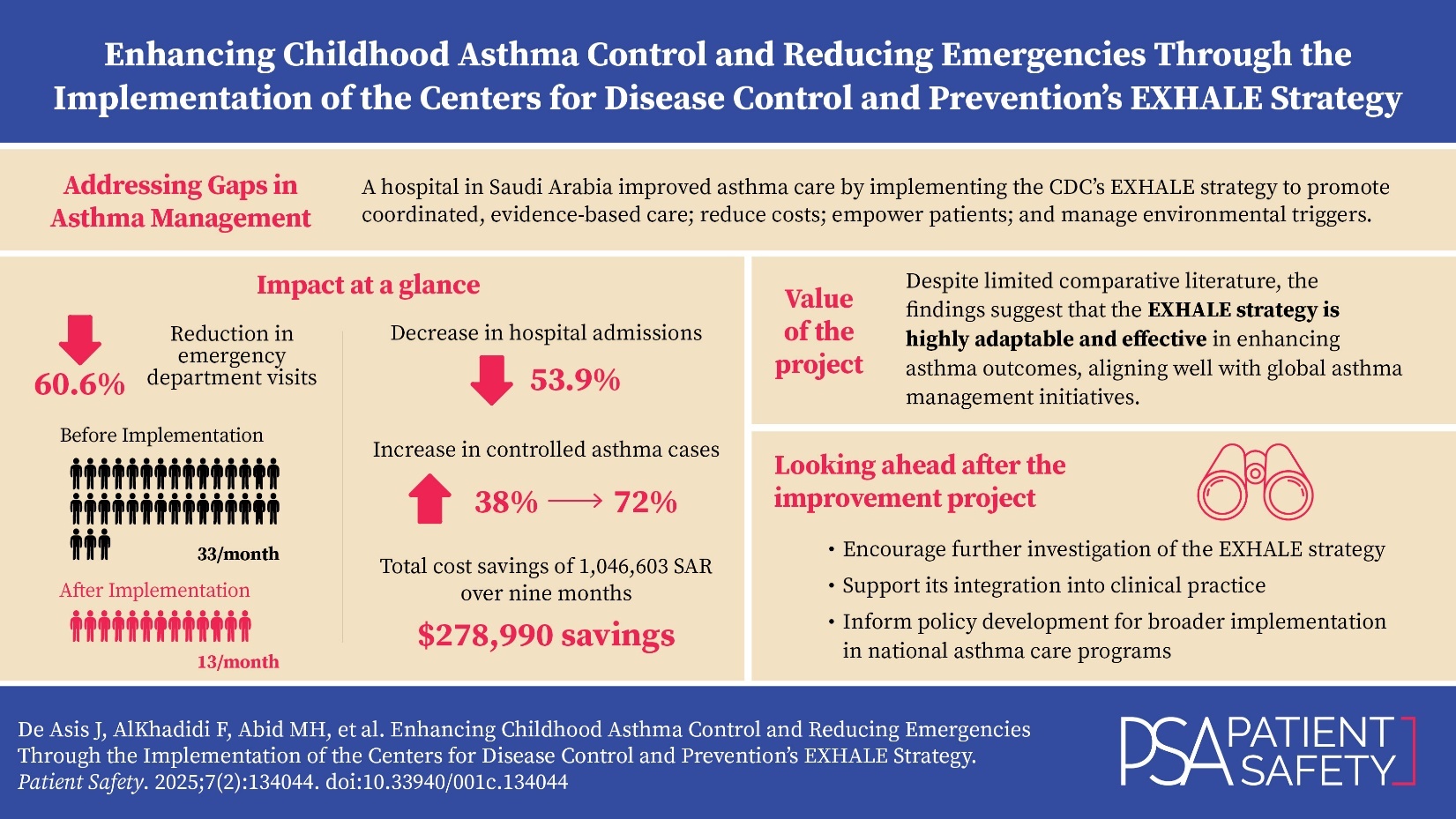
The strategy’s effectiveness underwent a thorough evaluation, involving the collection and validation of data related to asthma outcomes, processes, and balancing measures (Figure 2). This systematic approach allowed for a detailed analysis of the strategy’s influence across five distinct outcome measures and the assessment of the effectiveness of six implemented processes.
Emergency Department Visits
The primary outcome of the project was the targeted reduction in ED visits related to asthma exacerbation. The monthly average visits were reduced from 33 in the pre-project phase to 13 during the project implementation phase (Figure 3). Therefore, the targeted reduction in ED visits related to asthma resulted in an approximate 60.61% reduction in monthly average visits.
Asthma-Related Hospitalizations
The average monthly admission rate decreased from 13 patients to 6 patients (Figure 4). Therefore, the reduction in the average monthly admission rate was approximately 53.85%.
Percentage of Controlled Asthma Patients
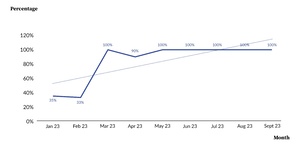
Shown in Figure 5, there was a substantial increase in the average of controlled asthma from 38.33% in 2022 to 72.44% during the project implementation.
Operational Gains (Healthcare Cost Reduction)
Saudi Arabia’s healthcare system is government-funded and provided free of charge to all citizens and expatriates. The primary source of healthcare financing is the national budget, predominantly supported by the oil sector.10 Consequently, minimizing costs associated with the disease burden is crucial. Through our project, we achieved a 60.61% reduction in asthma-related ED visits and a 53.85% decrease in hospital admissions. These improvements translated into substantial cost savings of 1,046,603 Saudi riyals during the implementation period.
We decreased the financial burden of the asthma-related ED visits by 60.61% and admissions by 53.85%. This led to significant cost savings of 1,046,603 SAR throughout the project implementation. (Figure 6 and Figure 7).
Number of Asthma Patient Visits and Admissions
In the ED, there was a reduction from 295 visits in 2022 to 117 in 2023. In the pediatric ward, the number of visits decreased from 111 to 54. Similarly, in the PICU, there was a decline from 5 to 3 admissions. The OPD experienced a decrease from 744 visits in 2022 to 615 in 2023 (Figure 8).
The decline in the number of visits in OPD had a great impact on the TNAA, which refers to the third earliest appointment that is available for scheduling. The TNAA for 2022 was initially 23 days; however, following the project kickoff, there was significant improvement and the average TNAA decreased to 10 days (Figure 9).
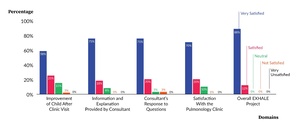
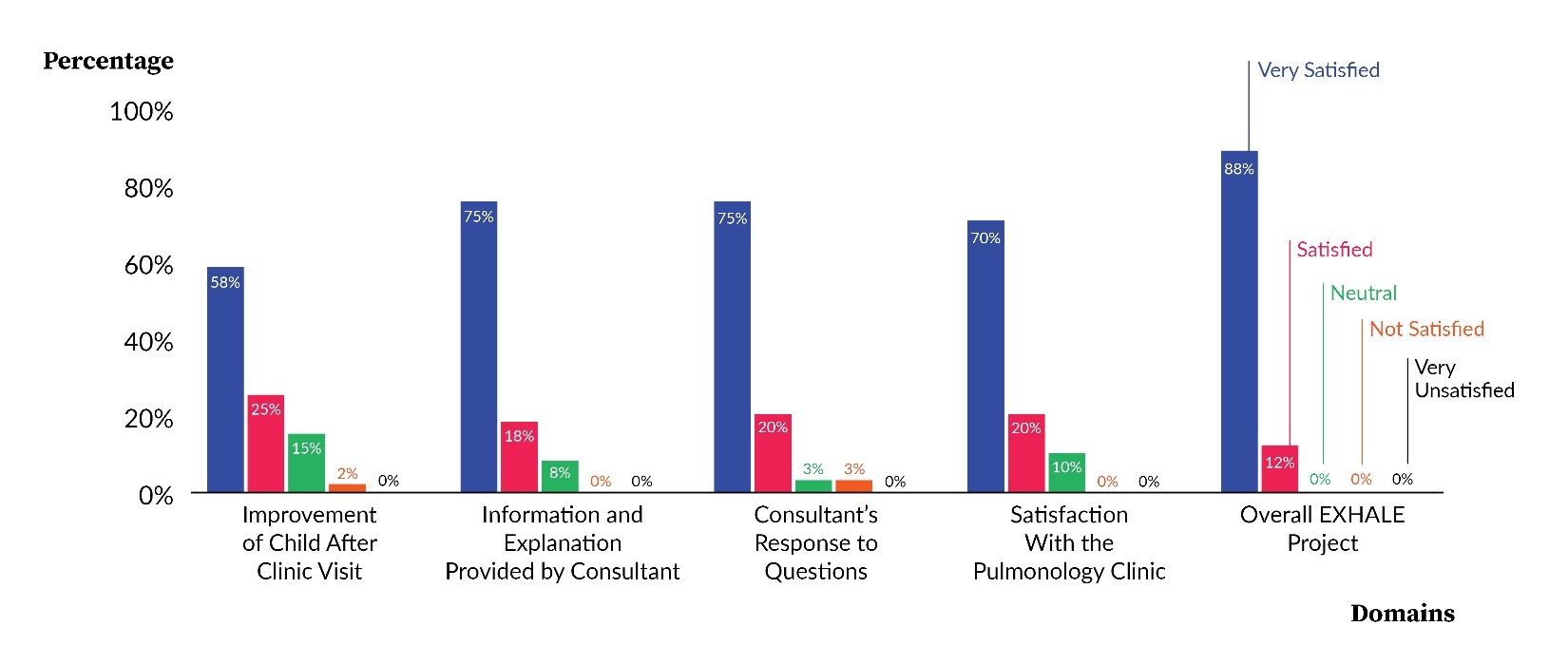
Patient Experience (Quality of Life Improvement)
The results from the Patient and Family Satisfaction Survey revealed an 88% for the overall project satisfaction (Figure 10 and Figure 11).
Average Compliance to Asthma Clinical Practice Guidelines by Physicians
The ED demonstrated an 82% compliance rate, the pediatric ward reached 86% compliance, and the PICU achieved 100% compliance (Figure 12).
Percentage of Compliance With OPD appointments
The team discussed the process measure involving compliance with OPD appointments (Figure 13), averaging at 73%, with administration. To enhance accessibility, especially for school-age patients, the team proposed initiating a virtual or telehealth program.
Unnecessary ED Visits
The process measure indicating the percentage of unnecessary ED visits is notably low at 1.6% (Figure 14).
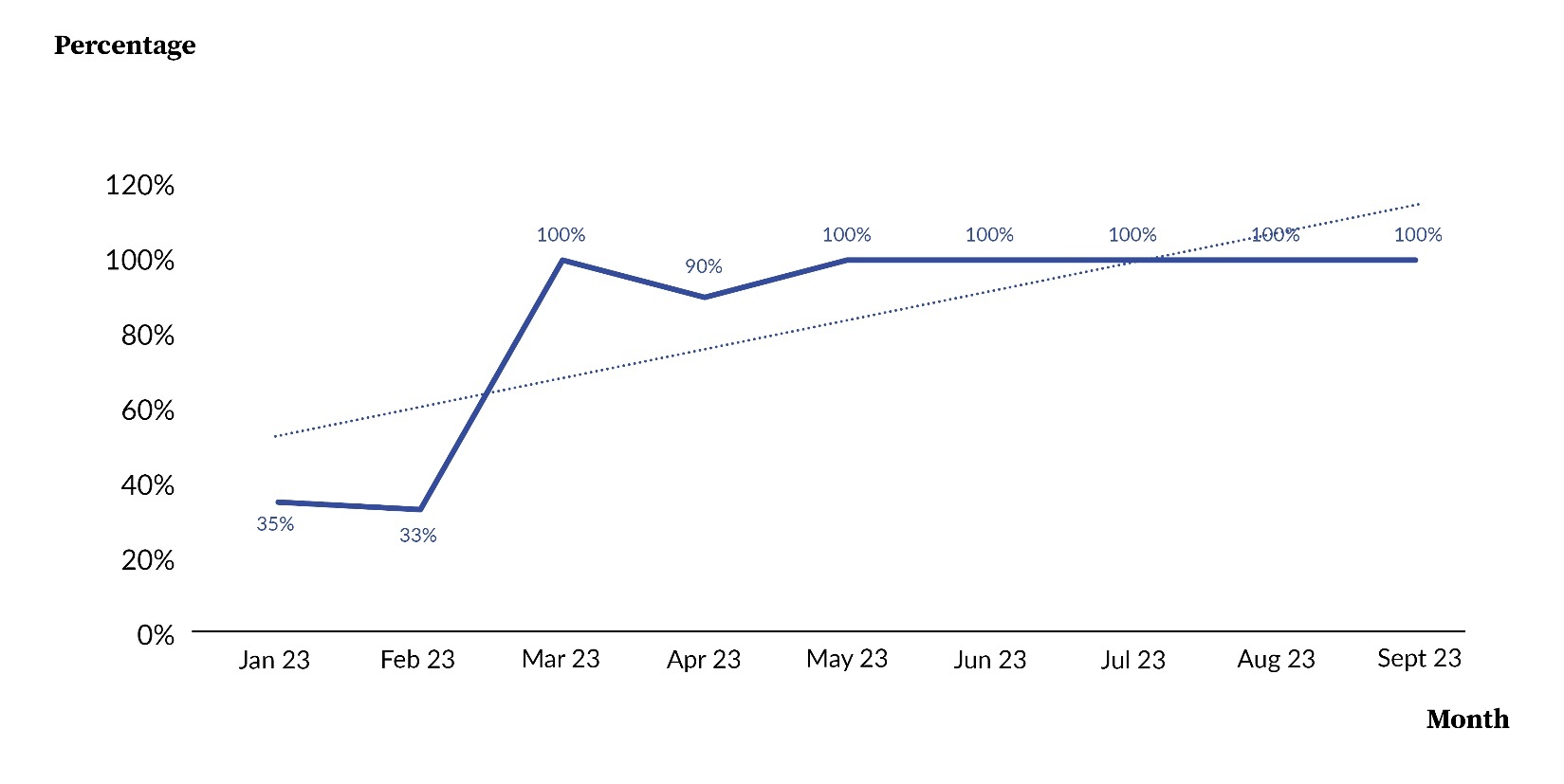
Patients Received Health Education About Asthma Management
The collection of data on patients referred to Health Education who received AS-ME measures the effectiveness of the strategy’s educational interventions. Initially, challenges were encountered, as health educators were not strategically integrated into the team and the team received no training. However, during the second quarter, a strategic addition was made with the introduction of trained health educators (Figure 15).
Average Waiting Time to Receive Education From Referral
The average waiting time for referred patients to receive AS-ME in the Health Education Department indicates an average waiting time of 32 minutes in the OPD and 43 minutes in the pediatric ward (Figure 16).
Percentage of Correct Inhaler Usage
Shown in Figure 17, correct inhaler device use through return demonstration indicates an average of 96%.
Percentage of Correctly Diagnosed Patients
The collection of the percentage of correctly diagnosed patients served as a balancing measure for our project. In the ED, the average correct patient diagnosis reached 96%. Similarly, the pediatric ward demonstrated accuracy of 98%. The PICU attained 100%, signifying precise diagnoses in critical care scenarios. Additionally, the OPD achieved a 100% accuracy in patient diagnoses (Figure 18).
Summary
The EXHALE strategy in pediatric asthma management demonstrated significant success, including a remarkable 60.61% reduction in ED visits; a 53.85% decrease in monthly admissions; and a substantial improvement in controlled asthma, rising from 38.33% to 72.44%. The percentage of controlled patients increased from 38% to 72%. Additionally, the implementation led to a commendable cost reduction of 1,046,603 SAR from January to September 2023, highlighting the strategy’s success in improving healthcare efficiency and patient outcomes.
The positive impact on process measures further reinforces this success, with a 73% compliance rate with OPD appointments, CPG compliance of 89%, unnecessary ED visits reduced to 2%, and an effective education rate of referred patients about AS-ME. Further, the low 1.6% rate of unnecessary ED visits contributed to the overall positive outcomes.
In terms of balancing measures, correct patient diagnosis resulted to an average of 98.5%. Overall, the EXHALE strategy has demonstrated comprehensive success in pediatric asthma management, including positive clinical outcomes, cost reduction, and accurate patient diagnoses.
Discussion
Interpretation
The outcomes of the implemented EXHALE strategy stand strongly with the CDC’s principles for pediatric asthma management. The strategy’s significant reduction in ED visits aligns with the CDC’s emphasis on preventive measures and timely interventions to minimize acute asthma exacerbations.
Additionally, the outcomes of the EXHALE strategy distinctly align with fundamental healthcare quality domains, underscoring its impact on pediatric asthma care. Firstly, for the safety domain, our project’s impact on the reduction in ED visits and admissions and maintaining an average patient diagnosis accuracy of 98.5% ensures safety and commitment to patient well-being. Effectiveness is evident in enhancing controlled asthma cases, with an increase from 38.33% to 72.44%. Efficiency is addressed through a cost reduction of 1,046,603 SAR, emphasizing the strategy’s contribution to the efficient allocation and utilization of resources within the healthcare system. The patient-centeredness is evident in high compliance rates with outpatient appointments and effective education about AS-ME.
The findings of our project align with and expand upon results from previous implementations of the EXHALE strategy in various healthcare systems. For instance, the Missouri Asthma Prevention and Control Program (MAPCP) achieved significant cost savings by integrating AS-ME and environmental assessments into Medicaid-reimbursed services.13 Their focus on increasing guideline-based medication use aligns closely with this project’s emphasis on clinical guideline adherence, with similar reductions in healthcare utilization.
Throughout the project’s duration, the implementation of the EXHALE strategy has yielded positive outcomes for the ongoing patient flow “ENSIAB” project in the OPD, particularly within the Pediatric Pulmonology clinic. The reduction in TNAA wait times from 23 days to 10 days underscores the strategy’s effectiveness in enhancing the efficiency and responsiveness of healthcare services, aligning seamlessly with the patient flow project’s objectives.
Limitations
The EXHALE strategy, while successful in achieving positive outcomes, is not without its limitations. One key limitation is the potential variability in the implementation of the strategy across different healthcare settings. The success observed in this particular context may not necessarily be replicated in diverse settings with distinct patient populations and healthcare infrastructures. Additionally, the reliance on self-reported measures, such as patient satisfaction and compliance, introduces the possibility of social desirability bias and may not fully capture objective indicators of the strategy’s impact. Another limitation is the dependence on historical data for comparison, which may not fully account for external factors influencing outcomes over time. Furthermore, the study’s duration may limit the assessment of the strategy’s long-term sustainability and its adaptability to evolving healthcare landscapes. Despite these limitations, the EXHALE strategy serves as a valuable initiative in pediatric asthma management, and ongoing evaluations and adaptations can address these challenges for continuous improvement.
Conclusions
The success of the EXHALE project extends beyond qualitative measures, encompassing significant enhancement in the quality of life for asthmatic patients. The project’s multifaceted approach, incorporating game-changing ideas, teamwork, training, and patient engagement, has resulted in a transformative impact on the overall well-being of individuals living with asthma.
By adopting patient-centered strategies, the EXHALE project addressed not only the medical aspects of asthma management, but also the broader aspects of patients’ lives. The emphasis on education, awareness, and self-management empowered patients to take an active role in their health, fostering a sense of control and confidence in managing their condition. As a result, patients experienced fewer asthma attacks, improved symptom control, and better overall respiratory health.
Disclosure
The authors declare that they have no relevant or material financial interests.
Data Statement
The authors confirm that the data supporting the findings of this study are available within the article.
About the Authors
Jean Barrientos De Asis (jeandeasis07jed@gmail.com) is a registered nurse licensed in the Philippines, Saudi Arabia, and New York. She holds bachelor’s degrees in biology and nursing, along with a Master of Arts in nursing. De Asis is also a Certified Professional in Healthcare Quality (CPHQ) and a Lean Six Sigma Master Black Belt. In her current role as a nurse specialist specializing in emergency nursing, she actively contributes to advancing patient safety and participates in quality improvement projects at the Armed Forces Hospital Taif Region.
Fawzyh AlKhadidi is the regional Pediatric Department director at the Armed Forces Hospital Taif Region. She also serves as a pediatric pulmonary consultant and the head of the pediatric pulmonary subspecialty. Dr. AlKhadidi leads the quality improvement project featured in this publication, driving advancements in patient care and clinical outcomes.
Muhammad Hasan Abid is the regional head of Patient Experience & Continuous Quality Improvement and Patient Safety specialist physician at the Armed Forces Hospital Taif Region (AFHTR). He is also an Institute for Healthcare Improvement fellow, mentor, and subject matter expert. He provides leadership and strategic alignment of the quality improvement and patient safety projects with the strategic goals for patient experience at the AFHTR.
Turki AlOtaibi is a registrar physician at the Armed Forces Hospital Taif Region. He champions the EXHALE strategy in the general pediatric ward, contributing to improved patient care and outcomes.
Jamal Mousa Alnofeye is a healthcare executive and quality leader with extensive experience in Saudi Arabia’s healthcare sector. As director of Quality and Patient Safety at Taif Military Hospitals, he drives strategic planning, accreditation, and patient safety initiatives. A board member of the Taif Health Cluster, he has also contributed to national healthcare policies. With degrees from Harvard Medical School and King Abdulaziz University, Alnofeye combines clinical expertise with strategic leadership, publishing research and leading quality improvements to enhance patient care.
Mohammed Althobaiti is a registrar physician at the Armed Forces Hospital Taif Region. He champions the EXHALE strategy in the emergency department-pediatric zone, contributing to improved patient care and outcomes.
Abdulrahman AlHazmi is a registrar physician at the Armed Forces Hospital Taif Region. He champions the EXHALE strategy in the Pediatric Outpatient Department, contributing to improved patient care and outcomes.
Hasan H. Althumali holds a diploma in respiratory therapy, as well as bachelor’s and master’s degrees in healthcare management. He currently serves as the regional director of Health Education at the Armed Forces Hospital Taif Region.

.jpeg)
_vs_2023_(project_implementation).jpeg)
.jpeg)
_.jpeg)
_vs_2023_(project_implemen.jpeg)

.jpeg)
.jpeg)
.jpeg)
.jpeg)

.jpeg)
.jpeg)

.jpeg)

_vs_2023_(project_implementation).jpeg)
.jpeg)
_.jpeg)
_vs_2023_(project_implemen.jpeg)

.jpeg)
.jpeg)
.jpeg)
.jpeg)

.jpeg)
.jpeg)