Introduction
Problem Description
Multiple medication discrepancies were submitted to the patient safety event reporting system (PSERS). It was discovered that these patients did not receive one or more doses of an important medication on admission. Those medications were on the discharge medication list from prior facilities but were not ordered on admission. In each case, the admission medication reconciliation (AdmMedRec) tool in the electronic health record (EHR) was either not used or incorrectly used.
Setting
This project was conducted at a standalone facility within a large academic medical system, which houses a 58-bed inpatient rehabilitation facility (IRF) and an 18-bed long-term acute care hospital (LTACH), collectively referred to as “post-acute care facilities.” The IRF is staffed with resident physicians and advanced practice practitioners, while LTACH patients are cared for by hospitalists.
Available Knowledge
Medication errors, particularly during care transitions, are responsible for 60% of all errors in hospitals.1–3 Medication discrepancies during transfers from hospitals to post-acute care facilities are associated with adverse patient outcomes.4
The AdmMedRec process begins with curation of a single, up-to-date list of medications that a patient is taking or should be taking from all available sources.5 Once the prior-to-admission (PTA) medication list is updated in the EHR, a provider then makes a clinical judgment on whether to continue, hold, substitute, or discontinue each medication based on clinical appropriateness and formulary availability.
The best available medication history can be gathered in a multitude of ways: speaking with the patient or family about their medications, referring to the patient’s discharge medication list from the hospital, hand-off communication when a patient is transitioning to a new level of care, utilizing the pharmacy dispense report, and viewing historical medications in the EHR. Appropriate use of these five sources to review and reconcile a patient’s medication list can decrease the number of medication errors during transitions of care.6
Background
Many hospitals struggle with AdmMedRec completion due to limited physician engagement or lack of perceived value.7 Successful interventions have either used “hard stops” or pop-up alerts in the EHR to prevent or interrupt order entry until AdmMedRec was complete.8,9 However, such EHR implementation can be disruptive to workflow and dissatisfying to providers. Designing clinical decision support in the EHR can also be a time-consuming process in a large health system that requires consensus building through various levels of governance structure. Other strategies relied heavily on embedding pharmacists in the admission workflow,10 which could be costly and difficult to scale.
Our hospital identified a series of errors related to AdmMedRec. These errors included medications not being ordered upon admission or ordered with an incorrect dose or frequency. We used failure mode and effects analysis (FMEA) to understand the AdmMedRec process and analyze these safety events. In the information-gathering phase of the FMEA, it was discovered that the admitting providers were primarily responsible for completing AdmMedRec. Pharmacy had limited resources to routinely review medication orders upon admission and compare them to the discharging hospital medication list for accuracy.
We then analyzed the medication events. A fishbone diagram was created to identify key contributing failures (Figure 1). It was discovered that there was no standard process for completing AdmMedRec, and providers were either not using or incorrectly using the medication reconciliation tool within the EHR. Additionally, it was noted that providers received limited formal education on medication reconciliation as part of their clinical or EHR training. Most providers reported learning from their peers, and not all followed the same process. They also depended on the admission liaisons to provide medication information from referring hospitals, which was often outdated by the time of patient arrival.
Existing Process
Due to the large number of daily admissions, providers at the post-acute care facilities would routinely initiate admission orders prior to patient arrival. They would start the process by reviewing the medication data from the preadmission packets compiled by the admission liaisons and saving orders in the EHR to be signed later into active orders when patients arrived at the facility.
Many providers entered individual medication orders directly without first compiling a single PTA medication list or using the EHR reconciling functionality to order medications.
Patients who transitioned between facilities within the same health system shared a single PTA medication list in the EHR. Any changes to a discharge medication at the referring facility would discontinue the existing order and replace it with a new one. When these medications were saved in preparation for admission, the discontinued medication would disappear from the list of saved orders, while the newly replaced one would remain unreconciled.
As a result, providers either accidentally did not order an individual medication on the discharge medication list or failed to recognize when changes were made to that list from when the preadmission packet was compiled to the time of transfer.
Aim
Our goal was to reduce medication errors by developing and implementing a standardized process for AdmMedRec in the EHR using an iterative Plan-Do-Study-Act (PDSA) approach through improving education, standardizing workflow, and leveraging existing EHR functionalities without adding additional pharmacy resources.
Methods
Interdisciplinary Team
An interdisciplinary team was formed to address the issue raised in the FMEA and develop interventions to standardize the AdmMedRec process and reduce medication-related errors. The team included medical providers, pharmacists, a clinical informaticist, and a patient safety officer. One of the providers was identified as a provider champion.
Standardizing Workflow
Existing workflow was assessed to identify knowledge gaps and inconsistent practice. A step-by-step process for completing AdmMedRec was developed by the clinical informaticist and tailored to the patient population at the post-acute care facilities.
We leveraged the built-in but underutilized tools, such as patient list flags and admission checklists (Figure 2), collectively known in our EHR as the “required documentation feature,” into the provider workflow. A color-changing clock in the patient list column would visually indicate if one of the required admission tasks was incomplete. Providers could review the admission checklist report to see which task remained incomplete and click on the link to go directly to the activity.
Interventions
We developed interventions based on the key contributing factors identified in the FMEA (Figure 1). We followed a stepwise, iterative PDSA approach in the design and implementation of this project (Table 1).
PDSA Cycle 1: Education
A one-hour, case-based education session was developed for the providers at the IRF based on core competencies (Table 2) that we perceived to be necessary to complete AdmMedRec. The interactive session was developed by the clinical informaticist and delivered as a part of the required didactic curriculum for the residents. The session was attended by the medical director to convey the importance of this topic. Providers were shown how to add the required documentation column to their patient list, which was their default screen upon logging into the EHR, and how to access the admission checklist from that screen. As most health systems in the region used the Epic Systems EHR, a key component of the education was to learn how to query real-time patient care data, including their medication list, from the external facilities using Care Everywhere, a health information exchange (HIE) through our EHR vendor.
PDSA Cycle 2: Rounding and One-on-One Education
After the initial education, the provider champion on the project team met with the IRF providers to make sure they had the required documentation column added to their patient list and provided one-on-one support to guide them through a new admission.
PDSA Cycle 3: Tip Sheet
We expanded the project to the LTACH, where all providers are hospitalists who rotate through multiple hospitals within the health system. Given their rotation schedule and availability, we decided to create and disseminate education via email instead. They received general guidelines for AdmMedRec and a tip sheet for adding the required documentation column to their patient list view.
PDSA Cycle 4: EHR Dashboard and Weekly Emails
We created a dashboard in the EHR to allow real-time tracking of AdmMedRec completion status across all units. A designated member of the project team would review and send weekly email reminders to providers whose patients had incomplete AdmMedRec.
Data Analysis
We queried the PSERS to assess the frequency of medication-related errors on admission. We built reports in the EHR to track monthly AdmMedRec completion rates before and after each successive PDSA cycle. The AdmMedRec was considered complete when an action had been taken on every PTA medication by the time of patient discharge. We used AdmMedRec completion rates from July 1, 2022, to June 30, 2023, (FY23) as baseline. Four months of data were used for post-intervention comparison due to the late start date on the LTACH (PDSA cycle 3) so that the same number of months would be available for analysis. We used Fisher’s exact test to calculate statistical significance between pre- and post-intervention completion rates.
Results
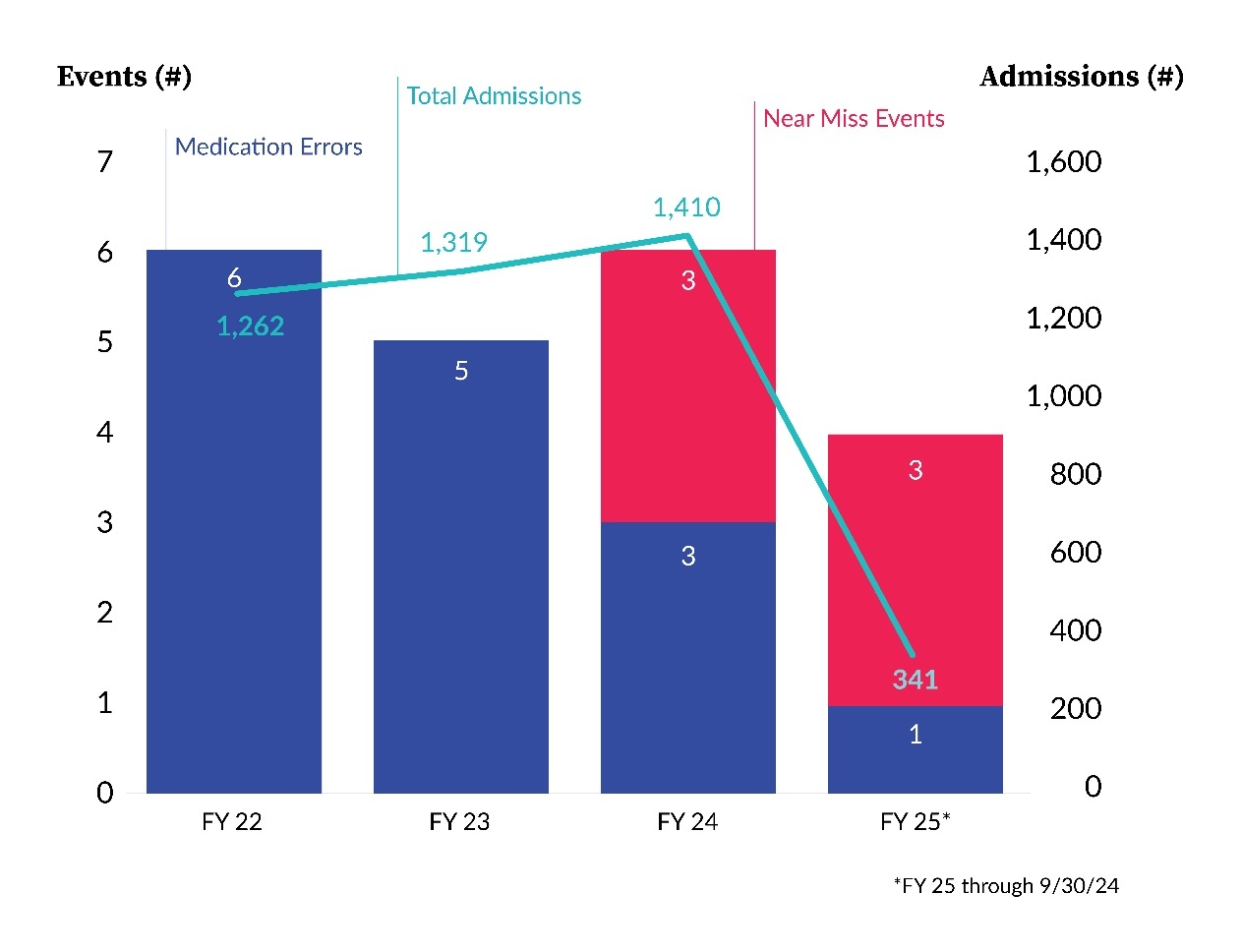
There were 1,319 admissions to the post-acute care facilities between July 1, 2023, and June 30, 2024, (FY24). A query of the PSERS found 5 reports of medication-related errors on admission in FY23 (Figure 3). There were 6 reports of medication-related errors on admission in FY24, of which three were near misses. In the first three months of FY25 (July 1, 2024, to September 30, 2024), there were only four cases of medication-related errors on admission, of which three were near misses.
The baseline completion rates for AdmMedRec in FY23 were 13% for IRF and 51% for LTACH patients. Significant improvements were observed on both units to 87% (p<0.00001) and 82% (p=0.001), respectively, in the four months after implementation (Figure 4).
Planning Phase (July 2023 to October 2023)
There was an initial increase in the AdmMedRec completion rate from 3% to 25% at the IRF in the three months after the FMEA. The standardized workflow was developed and informally socialized, but no formal education had been rolled out to providers during this time.
Cycle 1 (November 2023)
After the in-person education session was delivered to the IRF residents on November 1, 2023, there was a significant increase in AdmMedRec completion rate to 83% (p<0.00001) for patients who were discharged in November compared to baseline.
Cycle 2 (December 2023)
Continued improvement was seen in AdmMedRec completion rate to 92% after a one-on-one session with the IRF residents to guide them through an admission and make sure that they had the requirement documentation column added to their patient list.
Cycle 3 (March 2024)
Medication reconciliation guidelines and a tip sheet for the admission checklist were disseminated through email to the LTACH hospitalists. Their completion rate increased to 87% (p=0.0123) in March, compared to baseline (Figure 4).
Cycle 4 (May 2024 to June 2024)
There was a steady decline in the completion rate on IRF since December. After a real-time AdmMedRec dashboard was created, a weekly email reminder was sent out to providers who had patients with incomplete AdmMedRec. This resulted in a gradual increase in completion rate to 88% at the end of FY24 (Figure 5).
Discussion
The iterative implementation of a standardized AdmMedRec process with feedback mechanism significantly increased its completion rate. While the number of medication errors had decreased, the number of reported near miss events had increased (Figure 4). This was likely a reflection of an increased awareness of medication safety and provider engagement.
Previous studies have found varying successes through training.9 We postulate that our success was due to a curriculum that was tailored to the specific scenarios and challenges frequently encountered by providers at the post-acute care facilities. We believe that all three components of the workflow design are highly critical to its success. Providers must have the knowledge to perform the cognitive and technical tasks of AdmMedRec, have the visibility to the completion status in real-time, and recognize it as a priority in the organization’s culture of safety.
Overcome Initial Hesitancy
Time constraints and competing priorities were cited by providers as barriers to AdmMedRec. Providers were initially hesitant to change workflow due to perceived increase in the amount of time required to complete the admission process. The medical director participated in the PDSA cycles and was actively involved in reviewing and communicating the standardized workflow. His presence at the education session helped to impart the importance of this work as an organizational priority. Additionally, the one-on-one sessions not only addressed their perceived barriers, but also made the providers more receptive to the project aims.
Sustainability
There was a significant increase in the AdmMedRec completion rate immediately after the in-person education session, but we noticed a gradual decline in the subsequent months. While the session was part of the required didactic curriculum, due to rotation schedule, many residents were not on the inpatient rotation until several months later. The provider champion would check in with the new residents to make sure they had the required documentation column in the patient list view and follow the recommended workflow. While this required an initial investment in time, we believed that as residents became more familiar with the workflow, they would eventually serve as peer educators to help with the newer residents. We also built an operational support infrastructure with a designated person to review the real-time, unit-level AdmMedRec completion status and facilitate weekly email reminders.
Learning During the Project
Our initial assumption was that once AdmMedRec had been completed, the task would remain complete for the remainder of the hospitalization. However, we learned that any changes to the PTA medicine list, such as updates by a unit pharmacist, imports from external sources through HIE, or even modifications by outpatient providers within the same health system, would update the PTA medication list and render the AdmMedRec incomplete. Patients in post-acute care facilities within large health systems often have outpatient appointments during their hospitalization at a clinic that uses the same EHR. We felt that it was critical for providers to be aware of and acknowledge these changes. As such, we adjusted our target metric to AdmMedRec completion rate by hospital discharge to capture any changes that might have occurred during the hospitalization. It also reaffirmed the importance of our workflow design to incorporate the required documentation functionality to provide real-time, at-a-glance visibility of AdmMedRec status in the patient list view, without which providers would not easily find out when such changes to the PTA medication list had occurred.
Dissemination of Knowledge
The project team recognized that there was a significant knowledge gap in the cognitive evaluation of multiple sources of medication data, operational understanding of the different roles involved in the admission process, and technical proficiency in the EHR functionality. The case-based session was designed to specifically address common errors and misconceptions uncovered during the workflow analyses. However, this was a time-intensive process to develop tailored content and ensure availability of all providers. As we expanded our interventions to additional units, we strived to balance the benefit of an in-person session with both provider and resource availability. We decided to test whether education could be delivered via email, particularly for hospitalists, who we considered to be more experienced and generally more proficient in the EHR. They received AdmMedRec guidelines and a tip sheet describing how to use the required documentation functionality. We observed a significant increase since the implementation, although the effect was not as large, given the higher baseline. Longer-term data would be helpful to see if the improvement could be sustained over time.
Limitations
While we were able to significantly increase the AdmMedRec completion rate, it is important to recognize that we did not assess the accuracy of the medication orders. Accuracy was difficult to ascertain at scale without individual chart review and understanding of each patient’s unique medical history. Multiple factors might contribute to why a medication was changed at care transitions, some of which might be appropriate while others might not. Our hope was that as we fostered a culture of safety, there would be more mindful practice of safe medication management in the EHR.
Conclusions
An accurate medication list upon admission is vital to ensure correct medication orders. This rapid cycle PDSA quality improvement project successfully increased the AdmMedRec completion rate and reduced medication errors on admission.
The success was attributed to an interdisciplinary team developing a standardized AdmMedRec process tailored to the needs of the providers in the post-acute facilities within a large academic health system. We equipped the providers with the knowledge of how to perform AdmMedRec and a process that allowed them to have real-time understanding of its completion status.
The iterative process allowed us to rapidly respond to the learnings from each prior PDSA cycle and sustain the improvement observed since implementation. The successes of this project have stimulated interest to expand our learnings to additional units within the health system and changed how we provide onboarding training to new providers.
Acknowledgments
The authors would like to thank the medical director of the long-term acute care hospital, Dr. Gregory Mayro, and the chief medical officer of the Inpatient Rehabilitation Facility, Dr. Franklin Caldera, for their assistance and collaboration to implement this quality improvement project and support the sustainability of the project by educating and supporting the providers who complete admission medication reconciliation. The authors would like to thank Danielle Lenahan, pharmacy manager, and Joseph Galipean, pharmacy specialist, for their support and collaboration on this quality improvement project.
Disclosure
The authors declare that they have no relevant or material financial interests.
About the Authors
Kai Xu is a medicine consultant for the inpatient rehabilitation program at the Hospital of the University of Pennsylvania. He is an associate clinical professor of Medicine at the Perelman School of Medicine and a core faculty in the Clinical Informatics Fellowship. Dr. Xu specializes in the implementation and optimization of electronic health records (EHR), as well as the evaluation and integration of emerging technologies to transform clinical care and enhance patient experience. He has played a pivotal role in developing institutional guidelines for EHR usage, optimizing clinician workflow, and standardizing clinical care practices. His expertise extends to performance improvement methodologies, with a focus on advancing quality of care and patient safety.
Nina Renzi (nina.renzi@pennmedicine.upenn.edu) is a nurse with over 30 years of experience in various specialties. She is the director of Patient Safety, Risk, and Regulatory at Good Shepherd Penn Partners (GSPP) Rehabilitation and serves as the patient safety officer. Renzi earned her nursing diploma in 1993 and a Bachelor of Science in nursing in 2013. She is currently pursuing a juris master’s in health law. Renzi is certified in patient safety and healthcare risk management. At GSPP Rehabilitation, Renzi focuses on enhancing patient safety by identifying and analyzing adverse events. She implements measures to prevent future incidents, ensuring continuous improvement in patient care standards.
Lauren Ragusa is a skilled and compassionate nurse practitioner with a diverse background in patient care. She began her healthcare journey by earning her undergraduate degree in nursing at Loyola University Chicago, followed by her Master of Science in Nursing degree with a focus on family medicine. With three years of experience as a registered nurse in orthopedics, trauma, and neurology, Ragusa developed a strong foundation in acute care and specialized medical fields. Building on this knowledge, she transitioned to the role of nurse practitioner and has now spent three years practicing in physical medicine and rehabilitation. Ragusa is deeply committed to helping patients recover and regain their quality of life through holistic, evidence-based approaches. Her expertise in both acute and rehabilitative care allows her to provide comprehensive, personalized treatment plans to address a wide range of physical conditions.