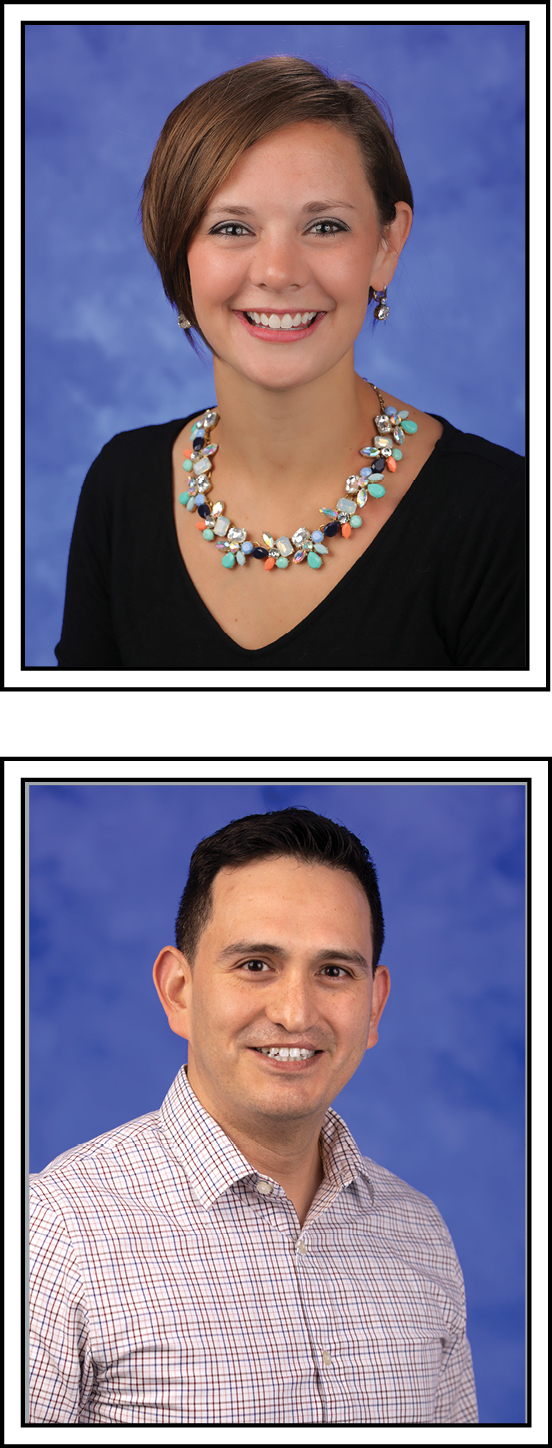
Executive Director’s Choice Award
Jesse Hixson, MSN, RN, Administrator
Allegheny Health Network Monroeville Ambulatory Surgery Center
In May, a patient was in the facility to have a procedure. When Jesse Hixson, the nursing leader, was made aware that this patient had been seen in a hospital for suicidal ideations, he took the patient to a quiet consult room to discuss that they were not going to have the procedure due to the hospital visit and medications that were given. The patient threatened him and the staff. Uncertain whether the patient had a weapon, Jesse de-escalated the situation and distracted the patient so they could alert other staff to call for help. He was barricaded in the room with the patient for almost 30 minutes to ensure that staff and visitors were safe behind the locked doors, until police arrived and apprehended the patient for transport to the hospital. Through this difficult and dangerous incident, Jesse remained clearheaded and proactive, going above and beyond to keep the patient, staff, and visitors safe. As a result, security systems were improved and on-site security has been provided.
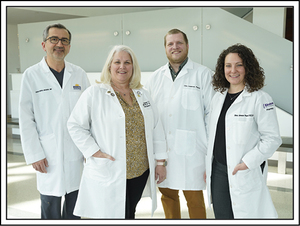
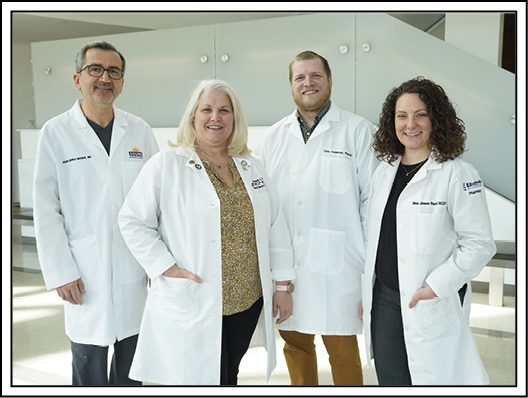
Sepsis
Jaber Monla-Hassan, MD, Olivia Johnson, PharmD, Christopher Anderson, PharmD, and Kim Mikula, MSN, RN
Einstein Medical Center Montgomery
Over several years, the Adult Intensive Care team worked on ensuring compliance with the three-hour and six-hour sepsis bundles. Despite ongoing education, optimization of a prescriber order set, and great compliance with various components, documentation of focused exams continued to be a problem.
The team posed a question of whether a smart notification could be built to fire when the sepsis order set was being signed in the electronic medical record. They worked with the technology department to implement such an alert; when fired, this notification not only reminds the provider but also opens the specific field for documentation. When the alert went live, providers were provided with education that explained the components of the three- and six-hour bundle, the order set’s design to help capture each element, and the importance of utilizing the order set when sepsis is identified.
Compliance with this element has improved from 66.7% in February 2022 to 100% throughout the first and second quarter of fiscal year 2023.
Ambulatory Surgical Facility
Mary Houton, Susan Walker, and the Ambulatory Surgical Center and Infection Prevention Registered Nurses
Penn Medicine Pennsylvania Hospital
The nursing staff at the Ambulatory Surgical Center and Infection Prevention (IP) teamed up to create a competency-based education collaboration. The team designed an infection prevention training program for healthcare personnel with measurable competencies for the observable knowledge, skills, and behaviors that one possesses to perform job responsibilities correctly and skillfully. To ensure that this education and training was translated effectively to practice, the team performed audits and encouraged feedback from staff. The goal of the education was to promote adherence with standards of care and help sustain effective practices.
Competency-based training is one of the key components to consider when designing an infection prevention training program for healthcare personnel and must be designed to meet the needs of a diverse group of learners. Key stakeholders included in the process were nurses, anesthesia, surgeons, surgical technicians, and surgical care associates. The observations included five areas of focus: surgical scrub technique, maintaining a sterile field, point-of-use instrument cleaning, traffic patterns in the operating room (OR), and room cleaning between cases. The observers assessed each component as either compliant or noncompliant. Benefits of this intervention include fostering a culture of safety, compliance, and interdisciplinary collaboration.
Number of observations per quarter:
-
Goal of 10 observations per OR location per quarter
-
Each observation includes the five areas of focus
-
Each area of focus contains five components that observers will assess as either compliant or noncompliant; clinical staff will have input to ensure observations are meaningful to practice
-
Areas of focus were chosen based on current competencies/policies and opportunities identified across the health system
Qualtrics audit form potential benefits:
-
Building relationships between OR clinical staff and IP department
-
Maintaining compliance and creating a culture of safety
-
Excellent opportunity for clinical nurses interested in quality improvement projects or looking to advance on clinical ladder
-
Successful standard process implementation can be translated to other areas of practice, such as the procedural areas (Interventional Radiology, Gamma Knife/Spine Center, Cardiology Services)
Results:
-
Observation period July 12, 2022, to August 2, 2022
-
117 observations made in each area of focus:
-
Surgical scrub (35)
-
Maintaining the sterile field (21)
-
Point-of-use instrument cleaning (23)
-
Traffic patterns in OR (15)
-
Room cleaning between cases (23)
-
-
Service lines observed: Ortho, ENT, Neuro, Breast, Colorectal Surgery, General Surgery, OB/GYN, Interventional Pulmonology, Vascular, Plastics, Urology, Ophthalmology
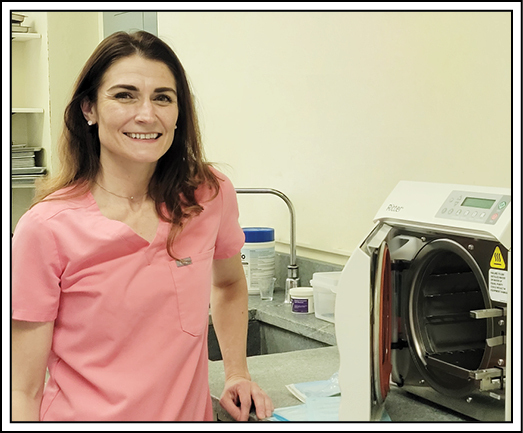
Long–Term Care Facility
Donelle Grove, RN, Infection Preventionist
South Mountain Restoration Center
Donelle Grove, RN, had worked at South Mountain Restoration Center as a floor nurse for many years, always interested in caring for her residents and learning new and better ways to do things. On January 1, 2022, she took over as the facility’s infection control preventionist and jumped into the role with both feet. She took the Advisory Committee on Immunization Practices (ACIP) training and passed on her first attempt. She used her class work to review and update several of the facility’s policies related to infection control, contributing to its increase to a five-star rating. Shortly after she came on board, she helped the facility navigate through an outbreak of COVID-19, during which only six residents became acutely ill—all on the same unit of 33 residents.
Grove took over coordinating COVID vaccine booster clinics, with 96% of residents having their primary series, 90% of residents having at least one booster, and 76% being considered completely up-to-date. She managed a recent flu vaccination clinic with more than 97% of residents accepting the flu vaccine and 98% of employees having received the vaccine or actively declined it. She has actively reviewed the vaccination status of all residents for pneumococcal, shingles, and hepatitis.
She has coordinated the sterilization of reusable equipment used by facility physicians and in the podiatry and dental clinics, and overseen the quality checks of sterilization equipment. She has provided training to staff on the use of personal protective equipment (PPE), glucometers, and maintenance and cleaning of the equipment.
Grove was instrumental in understanding the new Enhanced Barrier Precautions and assisted in developing the necessary policies and procedures. She upgraded the management of PPE supplies on the units for efficiency and accountability to allow the implementation of the Enhanced Barrier Precautions and efficient deployment when the need arises for acute infections.
In short, she has had a major impact for the better on the facility’s ability to maintain patient safety and an environment free of infectious disease.
Transparency and Safety in Healthcare
Behavioral Health 6 Spruce Shared Governance
Penn Medicine Pennsylvania Hospital
Upon arrival to an inpatient unit, there are times when the disorganized behavioral health patient is extremely ill and cannot answer questions surrounding naming the people that they would like to get information about them. Sometimes there are many people that care about the patient, family members or peers, who may call multiple times a day for information on how the patient is doing. The Behavioral Health Shared Governance team saw an opportunity to collaborate on creating a process that would enhance communication while also keeping patients safe. The result was the creation of a patient/family satisfaction form.
They asked both the patient and their family questions about the most important information that would help them feel good about the care being received and what times would work to make sure that they got this information. The team decided that there should be some type of identifier: the patient giving consent and the names of two people they were OK with having information; in addition, the two support people would have an identifier to use when calling.
Once the patient can communicate and understand what was being asked, the unit clerk asks them to name two support people that they consented to getting information about their care. The patient is then told the last four digits of their medical record number (MRN) to provide to these support people, which is the identifier used when the support person calls the unit. Once the support people have been identified, the patient signs the form, the last four numbers of the MRN are placed at the top, and the names of the support people are written in. This stays in a binder at the unit clerk’s desk so that everyone knows who has permission to receive information.
Once a relationship with the patient and their support people is created, a registered nurse will speak to the support people about good times in the morning and afternoon to call the unit for information. These times are set up so that information can be shared with the least number of interruptions from external stimuli, such as medication administration, treatment team, and hand-off. Since implementing this process, staff have reported less-distressed calls from support people around their loved one’s care and that there is more confidence in knowing who the patient wants to receive information about them. The transparency around vulnerability and safety by the team surrounding safe, quality care is what made this project come to fruition.
Improving Diagnosis
Jung Yun, MD, Ryan Lee, MD, Peter Wang, MD, Meera Kasireddy, Terence Matalon, MD (Radiology Department), and Kevin Lo, MD (Internal Medicine Department)
Einstein Healthcare Network, Part of Jefferson Health
The Network serves an underserved population in which access to healthcare, including imaging, can be challenging. Traditionally, follow-up recommendations for imaging studies by radiologists were primarily initiated by the provider who ordered the original study. This team sought to improve compliance rates of these radiologist-recommended follow-up studies by also including the patient in the administration of their own healthcare.
In collaboration with a start-up software company, they helped develop and implement a natural language processing (NLP) algorithm and tracking-and-reminder system that identifies patients requiring follow-up imaging based on radiology reports, organizes follow-up recommendations by due date, and reminds patients of due or overdue recommendations via text messaging.
Patients were randomly assigned into control and intervention groups prospectively. Patients were deemed compliant with recommendations if exams were ordered, scheduled, or completed within a period spanning 30 days before and 60 days after the specified due date (the compliance range suggested by the American College of Radiology). The control group received no reminders during the study period. The intervention group received a reminder three weeks after the initial exam and up to three additional reminders after the due date (one reminder every two weeks). The compliance rate, or the percentage of compliant follow-up recommendations as defined above, was calculated for both groups.
The team analyzed a total of 268 outpatient radiology reports during the study period. The control group had a total of 179 recommendations and 54 noncompliant follow-up exams, for a 70% compliance rate. The intervention group had a total of 89 recommendations and 12 noncompliant follow-up exams, for an 87% compliance rate. This represents a 24% improvement (p=0.003) in compliance of recommended follow-up studies utilizing the automated software system of notifying patients compared to the baseline.
With this new workflow, the team demonstrated that implementation of an automated system that includes recommendation cataloging via NLP, follow-up compliance tracking, and patient reminder messaging can significantly improve rates of imaging follow-up and ultimately improve patient care and outcomes. As a result of this project, they have fully implemented this workflow to include all patients in the Network.
Safety Story
Suzanne Swift, 4 South, and Nancy Patterson, Professional Development/Med-Surg
St. Christopher’s Hospital for Children
Pediatric patients admitted with a new diagnosis of diabetes receive education to learn to safely care for their disease at home, which includes adding the number of units of insulin to prepare the proper dose. One patient and his mother could not grasp the concept of adding the appropriate numbers and often miscalculated the insulin dose. As an incorrect insulin dose could be fatal, there was great concern for this child’s return home, and a potential plan was made for medical foster care.
Nurses Suzanne Swift and Nancy Patterson knew there had to be a way to help this family stay together. They developed a simple addition sheet that formats the numbers to add the insulin dosages for blood sugar and amount of carbohydrates. The sheet includes a visual line for each dose followed by a plus sign, and finally the line at the bottom to indicate how much insulin the child should receive. They worked with the hospital’s special education teacher, Colleen Cerebe, to focus school sessions on this newly created insulin dose calculation sheet.
The sheet worked! For this patient and mom, it presented the information in a clearer and more concise manner, combining verbal and visual cues to make the dose calculation process safer. Although a seemingly simple concept, this newly created sheet was designed to help families with health illiteracy have a better understanding of their child’s treatment plan. The insulin dose calculation sheet has been used for many patients since this one and has made a huge difference for some families—enabling them to be go home with a confident understanding of how to care for their child’s diabetes.
Nationwide Warriors
Cyndi Brinkley
Riverside Walter Reed Hospital
Gloucester, Virginia
When the health system transitioned to a positive pressure, needless intravenous site connector, Cyndi Brinkley raised a concern about its design posing a high risk of spilling nuclear medicine when the syringe is removed. Such spills can result in unnecessary exposure and temporary shutdown of the room, delaying patient testing and care. The product representative confirmed this was expected and a change in technique may not avoid the risk. Supply chain leadership supported the safety concern and sent a neutral valve to be used with the at-risk nuclear med patients across the health system, until further evaluation can be conducted.
Individual Impact
Jenny Rex, MSN, RN, Nursing Professional Development Specialist, Pediatric Intermediate and Intensive Care Units, and Adrian Zurca, MD, MEd, Staff Physician, Pediatric Intensive Care Unit
Penn State Health Milton S. Hershey Medical Center
During routine rounds, a graduate nurse approached Jenny Rex and asked how staff would perform cardiopulmonary resuscitation (CPR) on a complex patient with severe spinal hyperextension. Given the shape of the patient’s spine, traditional CPR would not be possible. Rex immediately set to work exploring the literature and collaborating with the Simulation Center and Dr. Adrian Zurca to develop a plan to ensure the safety of this patient. They worked with the fabrication shop teams to design and create a custom backboard that would allow clinical staff to safely and effectively perform CPR for this patient.
Using X-rays and dimensions of the patient’s spinal curvature as a guide, the team created a 7 by 50 cm board with chamfered edges to prevent abrasion to both the users and the patient, with a hole at the top of the board for ease of handling. Once the board was created, they tested the methods of providing compressions with it in various forms. The team piloted various techniques while measuring effectiveness with an electronic CPR analyzer.
Once the most effective approach was identified, Rex developed a comprehensive training program to ensure all clinical staff who cared for this patient were proficient in the techniques needed to use the board effectively. The height of the bed needed to be adjusted to allow for the appropriate 90-degree angle and lateral approach to compressions, counterbalance was needed to prevent movement of the board during use, and staff needed to take a wide stance to ensure the necessary force was applied. Rex provided hands-on training to all nurse, respiratory therapy, and physician staff who could potentially be involved in a resuscitation event.
Weeks after development and training were complete, the patient required transfer to another facility for short-term specialized treatment. Rex contacted the clinical team at the receiving facility and provided virtual training on the use of the custom board. During the course of the patient’s treatment, there was a resuscitation event that required the use of the custom board and innovative CPR techniques. The clinical teams were able to quickly and effectively implement the methods they were taught by Rex, and the patient experienced a positive outcome.
Rex’s willingness to go above and beyond, think innovatively, collaborate with clinical and nonclinical teams, and keep the patient at the center of all she does ultimately saved this patient’s life. Additionally, because of this work, there is now a blueprint for all patients with severe spinal hyperextension to be provided safe and effective CPR when needed.
Physician Offices
Quality Department
OSS Health
With many surgeries being outpatient or inpatients being discharged within a few days after surgery, hospitals and ambulatory surgery centers can have a hard time identifying postop complications. A process was created between a hospital and the clinic where patients were seen for their postop visits for infection control surveillance, to identify postop infections. An opportunity to identify other postop complications or events was identified and merged with the surgical surveillance process. In this program, for three months postop surgeons’ staff ask every surgical patient a series of questions to identify postop complications. When the patient is roomed for the postop visit, the clinical staff ask patients about:
-
Urgent care, emergency room, or hospital visits since their surgery
-
Bleeding or blood clot issues
-
Medication reactions
-
Infection or wound healing issues or concerns
-
Swallowing issues
This information is reviewed by the surgeon who may need to provide treatment or interventions and is used for surveillance.
Patient Safety staff from the hospital where the surgery was performed review the information and if a patient answered yes, a more thorough chart review is done to determine if there was a postop complication. The data is reported to the Patient Safety Committee and/or the Infection Control Committee, as well as being available to the Surgical Department monthly, and is used to identify trends with infections, wound healing, postop deep vein thrombosis (DVT) and other issues. The hospital has both an operating room—where patients are admitted to the hospital, placed in extended recovery, or are discharged from the post-anesthesia care unit (PACU)—and an Ambulatory Surgery Center. The same process is used for both.
In the first 10 months of 2022, patients were asked the questions 16,715 times. For every surgical patient, on average they were asked the questions 3.35 times. One in every 26 postop patients responded with a yes to one or more of the questions. One in every 160 patients who were asked the questions had a postop complication or issue that was reported to the appropriate committees and departments for follow-up. One in every 522 patients who answered the questions was found to have a serious event.
Although this process is time intensive, it shows the organization’s commitment to patient safety and to identifying issues and improving patient outcomes. What started as a creative idea to capture surgical site infections has blossomed into a unique way to identify postop complications or issues that otherwise probably would have not been identified.
Time–Outs
Sara Frey, PharmD
Lehigh Valley Health Network
An order was placed for compounded sodium chloride 0.22% for enteral use for a 23-day-old infant. Pharmacist Sara Frey, recognizing the gravity of providing hypertonic saline to an infant who does not require it—including major fluid shifts and brain side effects—performed her own time-out after the solution was compounded and scanned appropriately. Upon visual inspection, she realized that the dispense prep computer program had a malfunction which allowed incorrect components to be barcode scanned without an error alert—and the order had been prepared using 23% sodium chloride instead of 0.22% sodium chloride. Had this solution reached the patient it would have barcode scanned for Nursing without error and could have resulted in serious harm to the patient. The dispense prep system was fixed so that this error does not occur again.
Runners–Up
Sepsis
Jenna Mastromarino Riley, Penn State Health St. Joseph Medical Center
Jefferson Health Sepsis Team, Jefferson Health
Ambulatory Surgical Facility
Adrienne Bellino-Ailinger, Einstein Endoscopy Center Blue Bell
The Direct Access Colonoscopy Team, Einstein Endoscopy Center Blue Bell
Long–Term Care Facility
Nicole Ross, Angela Borgo, Susan Bell, Kerri Brooks, Lynn Sauers, Jake Thieret, Douglas Zundel, Rachael Blank, and Lisa Painter and the UPMC Senior Living Multidisciplinary Team, UPMC Senior Living
Sugar Creek Station Managers, Sugar Creek Nursing and Rehabilitation
Transparency and Safety in Healthcare
Patient Safety Officers, Allegheny Health Network
Vicenta Gaspar-Yoo, MD, President; William Bailey, DO, Chief Medical Officer; Milissa Hammers, Chief Nursing Officer; Quality Safety Value Team (Patient Safety Officer, Regulatory Manager, Infection Control Nurse, and Quality Manager), Allegheny Health Network
Improving Diagnosis
Kara Mascitti, MD, MSCE, Medical Director, Healthcare Epidemiology and Infection Prevention; Alex Matika, PharmD, Pharmacist, Clinical Specialist; and Lauren Allen, PharmD, Pharmacist, Clinical Specialist, St. Luke’s University Health Network
Critical Care Unit, WellSpan Health York
Safety Story
The Operating Room Department at Forbes Hospital and Sara Angelilli, Allegheny Health Network
Beth Lindell, OR Manager, Allegheny Health Network Saint Vincent Hospital
Nationwide Warriors
Chrissie Blackburn, Project Patient Care
Vidya Saldivar, PharmD, Medication Safety Specialist; Mobolaji Adeola, PharmD, Medication Safety Specialist; and Archana Sadhu, MD, Chair of Diabetes Action Council, Houston Methodist Hospital, Houston, Texas
Individual Impact
Kristen Farrell, Oncology Infusion Center, St. Christopher’s Hospital for Children
Alyssa Tousignant, RN, BSN, Allegheny Health Network-Allegheny General Hospital
Physician Offices
Amy Coppersmith, WellSpan Health
Tiffany Irwin, Practice Coordinator, UPMC Hamot
Time–Outs
Emily Roth, BSN, RN, Oncology Nursing, Children’s Hospital of Philadelphia
Samantha Braverman, Einstein Medical Center Montgomery
Thank you to this year’s judges
Mike Bruno, MD, Penn State
Sophie Campbell, MSN, RN, PADONA/LTCN
Dan Degnan, PharmD, MS, Purdue University
Jackie Ewuoso, MPH, Betsy Lehman Center
Diane Frndak, PhD, MBA, Robert Morris University
Regina Hoffman, MBA, RN, Patient Safety Authority
Dani Jurgill, Patient representative
Stephen Lawless, MD, Nemours Children’s Health
Ariana Longley, MPH, Patient Safety Movement Foundation
Dwight McKay, Patient representative
Adam Novak, MA, Michigan Health & Hospital Association
Amelia Paré, MD, Paré Plastic Surgery
Marty Raniowski, MPP, PAMED
Veronica Richards, MD, Richards & Richards, LLP
Rob Shipp, PhD, RN, HAP
Stanton Smullens, MD, Retired
Eric Weitz, Esq., The Weitz Firm
About the Author
Eugene Myers (eugmyers@pa.gov) is the associate editor of Engagement and Publications for the Patient Safety Authority. He previously served as editor-in-chief of Communications, Office of Institutional Advancement, at Thomas Jefferson University and Jefferson Health. He earned his bachelor’s degree from Columbia University, is a graduate of the Clarion West Writers Workshop, and is an award-winning author of seven novels for young adult readers.
Disclosure
The authors declare that they have no relevant or material financial interests.

__and_the_ambulatory.jpg)









__and_the_ambulatory.jpg)