Introduction
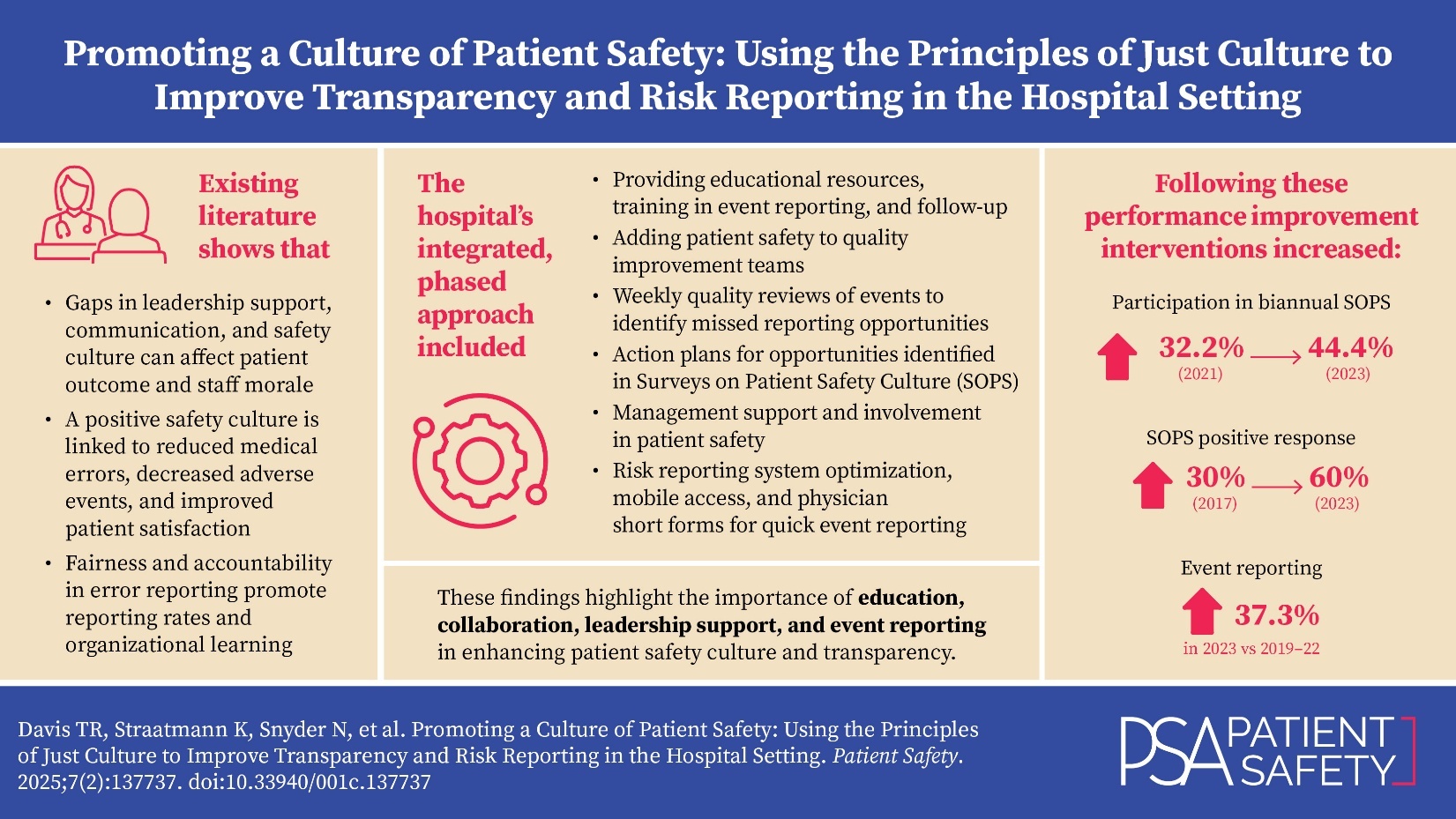
Patient safety is a cornerstone of quality healthcare, focusing on preventing harm to patients from medical errors or system failures. Despite its importance, healthcare organizations often struggle to cultivate a culture of safety and transparency. A 528-bed inner-city tertiary academic care center with over 4,000 employees faces similar challenges. The hospital conducts biannual Surveys on Patient Safety Culture (SOPS) via the Agency for Healthcare Research and Quality (AHRQ). While these surveys have historically low participation, they have shown opportunities involving leadership support, information exchange, and culture of patient safety. The hospital and its greater health system uses RL6 as its internal risk reporting system available to all staff. Historically, RL6 reflected a low reporting volume when compared to intersystem hospitals with similar or lower numbers of beds and staff, which validated the need for advancements in educational opportunities, transparent sharing of events and lessons learned, and improved safety culture.
The hospital’s challenges in patient safety culture and transparency have significant implications. With a participation goal of 60%, low participation rates in surveys (32.2% in the 2021 SOPS by AHRQ) and low RL6 reporting suggest gaps in leadership support, communication, and safety culture. These gaps can affect patient outcomes, staff morale, and the overall performance of the organization.1
Existing research underscores the importance of leadership support, communication, and a reporting culture in enhancing patient safety. Studies have shown that a positive safety culture is linked to reduced medical errors, decreased adverse events, and improved patient satisfaction.1 Moreover, the principles of Just Culture emphasizing fairness and accountability in error reporting have been shown to promote reporting rates and organizational learning.
The hospital’s need for interventions was guided by established frameworks such as the SOPS and the RL6 risk reporting system. Using these frameworks as a basis of improvement measurement, a multiphase project was developed. This project included educational initiatives surrounding resource updates, training, and follow-up; the establishment of quality improvement teams (QITs) aimed at enhancing patient safety culture and transparency; and leadership engagement.
This article looks to outline the implemented interventions, their impact on patient safety culture and transparency, and the insights gained for future initiatives. Improving patient safety culture and transparency is crucial for healthcare organizations like this hospital. By addressing the identified challenges and implementing effective interventions, the hospital aims to enhance patient safety, improve organizational performance, and provide better care for its patients.
Available Knowledge
In 1997, Lucian Leape, MD, testified to Congress that “the single greatest impediment to error prevention in the medical industry is that we punish people for making mistakes.”2 This testimony launched a new movement in healthcare, leading to the acceptance of a Just Culture. A Just Culture is a culture of learning, where staff trust they will not be punished for reported errors and accountability is accepted at all levels of an organization.3 In a Just Culture, human errors are not punitive and are recognized as unintentional and inevitable, leading to system examination and redesign, where the staff involved is treated with compassion.4
There are several barriers that make the creation of a Just Culture in the healthcare setting a challenging endeavor. A systematic review named trust as an essential aspect of a Just Culture and defined this as the belief in an error reporting culture that “is honest, safe, and dependable.” This review noted significant barriers to trust, including “lack of confidence in clinical skills, more fear of shame/blame by less experienced workers, and knowledge of the existing error reporting system” regarding users’ perception of event reporting.5 Voluntary reporting of patient safety events is vital to the sustainability of a Just Culture, and barriers to reporting can inhibit both the process and the success of a system.
A cross-sectional study utilizing historic data from the AHRQ SOPS Hospital Survey found common barriers to reporting were the lack of feedback on outcomes, action planning, or improvements following an event.6 In addition, the study found that punitive action toward errors significantly deterred voluntary reporting of patient safety events and can have a negative impact on the trust in an organization’s Just Culture.6 Other studies on organization safety culture have shown leadership barriers, including fear of management retaliation or no change due to reporting a patient safety error.7
The literature supports a variety of recommendations to help with implementing a sustainable culture of safety within healthcare organizations. Literature suggests that leadership engagement is crucial to setting the tone for an open and learning-oriented environment. It is recommended that leaders actively communicate and show their commitment to patient safety, thereby inspiring confidence among staff members. By engaging with frontline healthcare providers, leaders can bridge the gap between management and implementation, leading to more effective safety initiatives. In a Sentinel Event Alert issue published by The Joint Commission it is noted that leadership engagement encourages reporting.8 By building trust and encouraging reporting, leaders can empower staff to always be vigilant in reporting hazards despite the varying conditions faced in healthcare.8
Building trust is another crucial element in establishing a Just Culture. Research indicates that fear of retribution or punishment often prevents staff from reporting errors and near misses.9 To address this, leaders should create a culture of psychological safety where staff feel comfortable speaking up about potential issues without the fear of negative consequences. Trust, critical to shared accountability, can be fostered through transparent communication, active listening, and consistently addressing concerns raised by staff.9 In cultures of safety, staff routinely identify and report unsafe conditions and errors because they trust that their leaders want to know what is not working and will implement improvements with this information.9
Feedback can also play a critical role in the promotion of a Just Culture. Studies suggest placing priority on improving event feedback mechanisms and communication of event-related improvements made in response can increase the likelihood that a patient safety event will be voluntarily reported.6 Timely and nonpunitive feedback is crucial for staff to feel comfortable sharing their experiences. Leaders should actively engage with staff by providing feedback, recognizing their efforts, and highlighting the impact of reporting on patient outcomes. This process not only instills trust but also serves as a motivator for staff to continue participating in error reporting.
Commitment to the implementation of Just Culture is vital to sustaining Just Culture within an organization. Literature recommends the integration of safety practices into everyday processes, emphasizing that patient safety should be a core value within the organization.9 One example suggested for this is the implementation of an interdisciplinary team debrief following events to help destigmatize events overall.9 Collaborative debriefing following an incident helps in understanding the decision-making and identifying opportunities for system redesign.
In conclusion, Just Culture is crucial for fostering a climate that promotes error reporting and learning from near misses. Leadership engagement, building trust, feedback reporting, and commitment to implementation emerge as essential elements that contribute to the success of Just Culture. By actively incorporating these recommendations into healthcare organizations, leaders can create an environment where staff feel empowered to prioritize patient safety, resulting in improved outcomes for all.
Methods
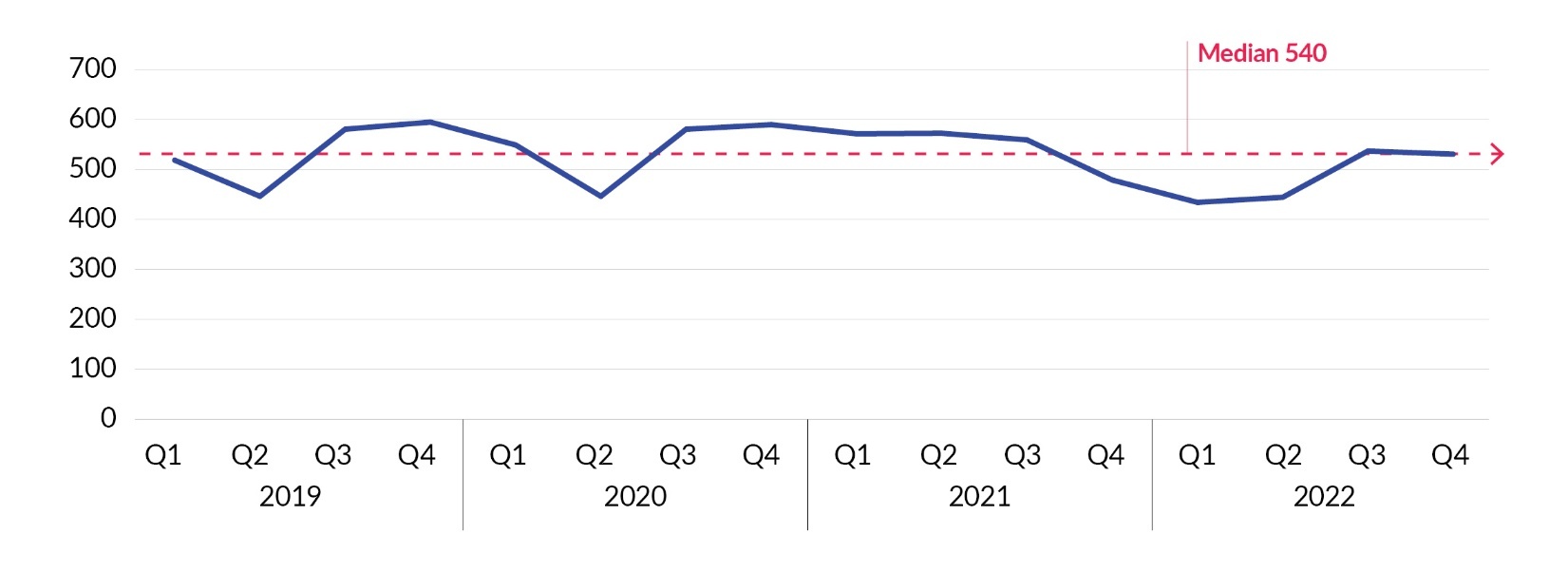
The study was performed at a 528-bed academic medical center serving low-income neighborhoods, with over 4,000 total employees. The biannual SOPS survey, electronically deployed to staff via email, in 2021 showed that less than half the hospital staff completed the survey. Lack of survey completion by staff was a concern; additionally, the survey results demonstrated that 56.3% of the staff had not utilized the patient safety reporting system, known as RL6, in the previous 12 months. Validating low staff incident reporting and a decreasing trend, the mean of patient safety events reported monthly ranged from 532 in 2019 to 485 in 2022 (Figure 1). Enhancing the culture of safety at this comprehensive academic medical center was identified as a priority goal for 2023 by the chief executive officer, chief medical officer, and chief nursing officer.
Key stakeholders, sponsored by the executive leadership team, were assembled in quarter 4 of 2022 to analyze gaps, review the latest evidence-based literature, and develop tactics to implement in 2023. They identified areas within the surveys as top-priority opportunities to improve the hospital’s culture of safety, including management support for event reporting, closed-loop communication regarding events reported, and a need for proactive reporting prior to the event reaching the patient (Figure 2). The team utilized The Joint Commission’s Robust Process Improvement (RPI) framework to guide change-management methods in a phased approach.
To enhance understanding, the team updated educational resources and shared them broadly. Detailed examples of what to report on in the RL6 system, required and recommended events by the Patient Safety Authority, were provided to all staff, utilizing a single-point lesson and educational sessions at hospital- and department-level meetings. For example, this education was provided during new-hire orientations, physician resident Quality Improvement and Patient Safety (QIPS) rotations, service departmental meetings, and hospital leadership meetings. To keep the focus on improving a culture of safety and creating continuing engagement, the team also presented at the monthly Quality Webinar Series and coordinated to educate staff and visitors during Patient Safety Awareness Week and national Healthcare Quality Week.
Phase I of the performance improvement began in January 2023. Phase I interventions included efforts to promote transparency in patient safety reporting with the goal of multidisciplinary collaboration and improvement in culture of safety. To share events with all levels of staff and within the multidisciplinary team, a patient safety component was added into the existing QITs within each physician institute. These teams include representation from physicians, nursing, Quality, Patient Safety, and multiple other disciplines as applicable to each institute. The Patient Safety team reviewed departmental-specific reporting and case reviews, providing a forum for open discussion and feedback. The QIT platform linked disclosure and system improvement, employed an integrated team approach to safety and transparency, and allowed for accountable review of opportunities and trends.
Phase II began in May 2023. Efforts to build upon the educational initiatives and progress in phase I, to promote accountability and sustainability, were implemented. The Quality team staff reviewed all mortalities, complications, readmissions, resuscitations, and other quality reviews for missed patient safety incident reporting opportunities. A weekly review of events was conducted collaboratively with the Patient Safety team and direct feedback and education was provided to nursing, physician, and operations staff. This partnership ensured identification of patient events, provided direct feedback to the units on reportable events, and ensured that documentation of events was captured within the RL6 risk reporting platform.
Phase III began in October 2023. In response to the results from the 2023 SOPS results, all hospital units and departments were requested to develop an action plan targeting their area’s top three opportunities identified in the survey. These action plans were to be monitored and updated at least quarterly for progress or barriers. Additionally, there was an overall hospital action plan approved and endorsed by senior leadership. This action plan was aimed at the hospital’s top three opportunities: staffing, work pace, and hospital management support for patient safety. Initiatives from the hospital action plan directly tying into this culture of safety project include management involvement in patient safety committee meetings, a 2024 rollout of a Just Culture algorithm, and optimization of the risk reporting system RL6. RL6 improvements included mobile RL6 risk reporting introduced to all staff in November along with the preexisting desktop access and a physician-specific short form for quick event reporting in December.
To evaluate the success of the phased initiatives to improve the overall culture of safety, a variety of reports and tools were utilized. To evaluate the staff perception of the hospital’s culture of safety, the SOPS results from 2021 and 2023 were compared and analyzed. Incident reporting practices and volume were captured within the RL6 incident reporting system and analyzed for statistically significant changes using R version 4.2.1 (R Foundation for Statistical Computing). Based on distribution of the data, a Wilcoxon signed-rank test and report medians and interquartile ranges (IQR) were used to analyze changes in reporting monthly compared to overall hospital patient days. Monthly data trending during the intervention was performed using a statistical process control chart to evaluate efficacy of interventions. And lastly, accountability and compliance with direct staff feedback and education from quality improvement reviews was captured and trended using a run chart.
Results
For the SOPS, the teams worked together to raise awareness during the education initiative and multilevel meeting presentations to improve participation of all hospital staff from 32.2% in 2021 to 44.4% participation in 2023. In addition, the SOPS results around “Leadership Response to Error” improved significantly, with the SOPS results showing a shift from a low positive response (30% in 2017) to a majority positive response (>60% in 2023). The Quality and Patient Safety teams’ improvements in transparency and collaboration resulted in a statistically significant 37.31% increase (p<0.001) in event reporting in 2023, despite concurrent increases in post-pandemic patient volume, compared to the average number of reports from 2019–2022 (Figure 3).
Positive increases in patient reporting by staff began in January 2023, corresponding with the inclusion of patient safety in QITs in January and in April when RL6 direct feedback began (Figure 4). Quality team review and staff feedback and education escalations peaked over the summer months, with an average of 30 escalations per month to reach a steady state of 10–11 escalations and reeducation of required RL6 reporting categories monthly by fall 2023 (Figure 5). Incidentally, the most notable increase in patient safety reporting was noted from December 2023 to January 2024, corresponding to an increase in laboratory leadership and team reporting patient safety events that were not previously captured. Management attendance in patient safety committee meetings improved from consistently less than 10 attendees to consistently more than 25 attendees after October.
Discussion
The project aimed to enhance patient safety culture and transparency at this hospital through education, collaboration, and increased reporting. Key findings include an increase in survey participation and event reporting, and improvements in leadership response to errors. These findings are relevant to rationale and specific aims, demonstrating the effectiveness of the interventions in addressing identified barriers.
The interventions were associated with positive outcomes, indicating a statistically significant association between the interventions and the improvement in patient safety culture and transparency. These results are aligned with findings from other publications that emphasize the importance of leadership support, education, and collaboration in enhancing patient safety.1 The project’s impact on people and systems was significant, with increased trust in the reporting system and a more open culture regarding error reporting, shown by the remarkable increase in risk reporting in RL6 (Figure 3). These outcomes suggest that the interventions may have been successful in changing attitudes and behaviors related to patient safety.
The results of this project are consistent with previous studies that have demonstrated the effectiveness of educational initiatives and collaborative approaches in improving a hospital’s patient safety culture.1 The findings also support the importance of leadership support and transparent communication in fostering a culture of safety.5 The project had a positive impact on both individual staff when reporting patient safety risks and the healthcare system in creating a positive feedback loop shown by the increased risk reporting and survey result improvements. The implementation of the various institute QITs facilitated multidisciplinary collaboration and improved communication, further enhancing the culture of safety.
The observed outcomes exceeded expectations, particularly in terms of increased event reporting and improved leadership response to errors in their participation with patient safety through the committee and the QITs. This may be attributed to the comprehensive approach taken by the project team, which included targeted educational initiatives, collaboration with key stakeholders, and regular feedback mechanisms. While the project required resources for implementation, including extensive Patient Safety and Quality teams’ time and educational materials, the long-term benefits in terms of improved patient safety and organizational performance outweighed these costs. The strategic trade-offs involved reallocating resources to prioritize patient safety initiatives, which proved to be a worthwhile investment.
An initial limitation of this project included low levels of staff engagement, particularly among the medical staff who were hesitant to encourage reporting due to legal or peer review implications. However, medical staff quickly adapted and supported the new level of transparency that the hospital and institute leaders led by example. A second limitation was the increase in reporting starting in December 2023, relating to the lab team RL6 submission volume, which exceeded the statistical process control limits as an outlier. Due to the outlier, efficacy of the RL6 mobile access and physician short-form risk reporting initiatives to promote ease of use will require more trending and evaluation. Another limitation of the project is its generalizability to other healthcare settings. The findings may be specific to the context and size of the urban academic medical center where the project was conducted. Also, while efforts were made to minimize bias and confounding factors, these limitations cannot be eliminated in a real-world setting.
Conclusion
In conclusion, the project successfully improved patient safety culture and transparency, shown primarily by improved survey results and increased event reporting, a core tenet of Just Culture. The interventions implemented were effective in addressing barriers to a Just Culture and promoting a more open, initiative-taking, and collaborative approach to patient safety. The sustainability of these improvements will depend on continued leadership support and ongoing monitoring and evaluation.
The teamwork by Patient Safety and Quality to employ an integrated approach to patient safety at this hospital resulted in improved transparency and advancement in the culture of safety. With strong leadership support, the 2023 SOPS results were broadly distributed and led to action plans to improve the culture of safety, which were targeted with clear, measurable goals and centered around encouragement of event reporting, improvement in report follow-ups, and learning from other units’ reports. To build on the success of this project, future efforts could focus on further enhancing the “Good Catch” program to encourage reporting of near misses and potential safety hazards. This could include the implementation of a reward system for staff members who identify and report potential safety issues and conduct regular audits to identify and address system-level issues. Additionally, ongoing education and training for staff members on patient safety best practices could help maintain a culture of safety over time.
Acknowledgments
Executive sponsors: Dr. Imran Qadeer and Marge DiCuccio; Medicine Institute sponsors: Dr. Marisa Evans and Dr. Thomas Walsh; Surgery Institute and Executive sponsor: Dr. Allan Philp; Cardiovascular Institute sponsor: Dr. Indu Poornima; Orthopedic Institute sponsor: Dr. Ryan Sauber; and Neurovascular Institute sponsor: Dr. Edward Prostko
Disclosure
The authors declare that they have no relevant or material financial interests.
About the Authors
Tanisha Davis (tanishardavis@gmail.com) is a registered nurse and United States Navy veteran with over 26 years of healthcare experience and has specialized as a quality improvement leader for the last 12 years. She has nursing specialty certification as a Clinical Nurse Leader (CNL) from the American Association of Colleges of Nursing and is a Certified Professional in Healthcare Quality (CPHQ). She completed her baccalaureate at Florida State University, her master’s degree at University of Pittsburgh, and doctor of nursing practice at Capella University.
Kathryn Straatmann (kathryn.straatmann@ahn.org) is a Certified Professional in Patient Safety from the Institute for Healthcare Improvement and brings a passion for patient safety through all her work in healthcare administration. With a baccalaureate at Saint Vincent College in biology and master’s in healthcare administration from Gannon University, Straatmann brings expertise to her current role in revenue cycle, which is rounded out by three years of experience in quality and safety work.
Nathan Snyder has a master’s degree in nursing from Capella University and is certified in patient safety. He spent eight years in an urban Level I Trauma Center in the emergency department and the last eight years working in patient safety with Allegheny Health Network. He has led projects to empower frontline staff and taught classes for hospital systems and Pennsylvania. His current focuses include improving culture, increasing reporting, and promoting a nonpunitive response to error.
Darcy Shiner is a registered nurse and quality improvement leader with over 14 years of experience in various healthcare settings, including critical care and clinical nursing, leadership, data analysis, and project management, with a strong commitment to evidence-based practice. She holds a Certified Professional in Healthcare Quality certification and completed her master’s in nursing administration at Waynesburg University.
Addie Evans is a registered nurse with over 20 years’ experience in healthcare. She completed her diploma of nursing at University of Pittsburgh Medical Center St. Margaret School of Nursing, baccalaureate at Ohio University, and master’s degree at Capella University. She also holds a Bachelor of Arts in women’s studies from the Pennsylvania State University.
Carla Caruso is a quality coordinator with 27 years of healthcare experience, including a decade with Allegheny Health Network. Her diverse background spans clinical and administrative roles in pediatrics, family medicine, imaging, and graduate medical education, culminating in her current focus on project management within quality, patient safety, infection prevention, and regulatory readiness. As a Six Sigma White Belt, Caruso is dedicated to enhancing patient care within the Quality, Safety, and Value Department at Allegheny General Hospital.
Maria Alton is a master’s-prepared registered nurse with a decade of diverse clinical and leadership experience, spanning orthopedics, neurology, trauma, emergency medicine, and nursing leadership. As a performance improvement specialist in the Quality Department at Allegheny Health Network, she leads data-driven initiatives to enhance clinical outcomes, patient safety, and operational efficiency. Alton earned an Associate of Science in nursing from Community College of Allegheny County, followed by a Bachelor of Science in nursing from Ohio University. In 2020, she completed a Master of Science in nursing informatics at Capella University.



.jpeg)



.jpeg)
